| Canine
Brucellosis
 319-320 319-320

Clinical signs
-
Clinical
signs may vary from none to mild.
-
Fever is uncommon because there is no
endotoxin to induce a fever.
-
The CBC is usually
normal, but there is a general lymphadenopathy because of the
reticuloendothelial cell stimulation. This may result in some spleen and
liver enlargement.
-
Other signs may include weight
loss, poor hair, listless attitude. Some classic
signs include thoracic or lumbar diskospondylitis, and endopthalmitis
and uveitis caused by immune complex deposits in the eye.
-
In
the female ABORTION at 30-50 days of normal-partly autolyzed pups, or
live and stillborn pups. The bitch is bacteremic 2-3 months, but
otherwise healthy, even though a vaginal discharge may be present.
-
A
bitch may lose 2-3 litters in succession. It may
appear that INFERTILITY is a problem as early embryonic death may occurr
at 20
days, or fetal resorption produces focal necrosis of chorionic villi and
bacteria in trophoblastic epithelial cells.
-
Signs
in the male may also include infertility as well as epididymitis,
orchitis, and scrotal dermatitis that results from scrotal licking due
to orchitis.
-
Testicular atrophy and
azoospermia may be seen.
-
Up to 90% sperm
abnormalities, head to head sperm agglutination, sperm phagocytosis, and
PMN's and monocytes in the semen.
Transmission
-
Transmission is
primarily venereal and oral (i.e through the mucous membrane)
-
There
are 2 X 106
colony forming units in an infective dose and 1010
organisms /ml in the discharge, which means there are 500 infectious
doses/ml.
-
The discharge may continue for 4-6 weeks post abortion.
-
The semen only has high numbers of bacteria for 1-2
months, but the disease spreads via the semen anyway.
-
Kennelmate
to kennelmate transmission was not seen experimentally when dogs of the
same sex were housed next to each other for 10 months. Therefore urine
and indirect mucous membranes contact are not important routes of
transmission.
-
The aerosol route is only important if conditions are
crowded. The milk may contain the organisms.
Pathophysiology
-
The bacteria
attaches to the mucous membrane and penetrates, with more attachments
increasing the virulence.
-
There is a bacteremia that starts 20 days post
exposure and the bug spreads to the lymph nodes and is transported to
reticuloendothelial cells, prostate, uterus, and placenta.
-
It grows
intracellularly in steroid sensitive tissue mostly.
-
The animal then
become a source of bacteremia with episodes that last for years.
-
In
males there is epididymitis, and sperm leakage that causes antisperm
antibodies to develop.
-
In the bitch there is a
placentitis, whose exact mechanism is unknown.
Recovery
-
Spontaneous
recovery can occur 1-3 years post infection, followed by a decrease in
the titer.
-
The titer does not rise again if the animal is challenged and
re-infection does not occur because cellular immunity is most important.
Diagnosis
-
Culture from the
blood, lymph nodes, marrow, urine, milk, vaginal discharges or semen is
the only definitive diagnosis.
-
Experimentally the organism was seen in
100 % of the dogs at 2 months post infection and the bacteremia lasted
6- 12 months.
- The organism was recovered in 100% of the males, and 30%
of the females in tissues (lymph node, spleen) when they were
abacteremic.
Rapid Slide Agglutination Test (RSAT, 'Card Test')

- The RSAT uses B. ovis bengal stained antigen
because it just works better than B. canis antigen.
- The test is performed by mixing the antigen with
the patients serum. A precipitate means the test is positive.
- There can be as high as a 60% false positives
because of Bordatella, Pseudomonas, Moraxella, B. ovis titers.
- The test becomes positive 2 to 8 weeks post infection
and remains positive 40 to 60 months post infection.
- False negatives are very rare. One scenario you may
see is a 'false negative' when the recently infected bitch is less
than 8 weeks into the disease and the titer has actually not yet
become positive.
- Otherwise, a negative test is usually indicative of
a negative dog.
- If the test is positive, further testing is needed
because of the high incidence of false positive tests.
2ME-RSAT
- This test is the same as the RSAT except
mercaptoethanol is added to eliminate nonspecific binding of 19S
agglutinins, although it too may not be accurate.
Tube Agglutination Titer (TAT)
- In this test B. canis antigen is diluted and sera
is added to determine the titer.
- If the titer is greater than 1:200, it is positive
and 1:50 to 1:200 is suspicious.
- This becomes positive 4-8 weeks post infection and
then becomes negative 40-60 months post infection.
2ME-TAT
- Same as TAT except 2ME added and there is
practically no difference in sensitivity
Agar Gel Immuno Diffusion (AGID) using the cell
wall antigen
- This test becomes positive 8-12 weeks post
infection and becomes negative 40-50 months post infection. When the
bacteremia stops, the titer declines.
AGID using the cytoplasmic antigen
-
This test becomes positive 8-12 weeks post
infection and did not become negative for 64 months (lifelong) post
infection experimentally.
-
This test is very specific for
Brucella sp., and a positive test is used diagnostically to confirm
RSAT positive tests.
Summary of diagnosis
-
Use the RSAT, 2ME-RSAT to screen
and identify all negative animals.
-
Use the AGID cell wall antigen
test to confirm the disease.
-
Culture is the only definitive
diagnosis and is the best diagnostic test in the first 2 months of
the disease, however dogs become abacteremic after 27-64 months.
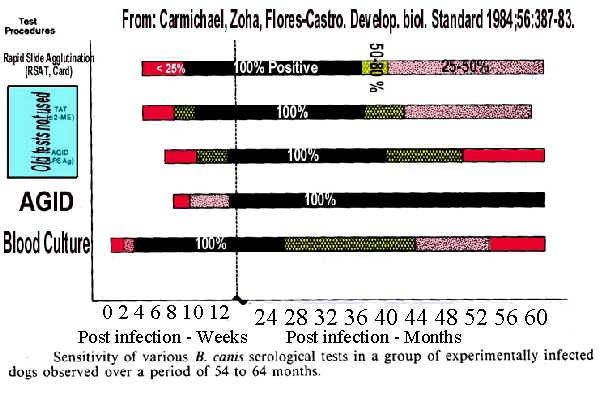
Click the graph to enlarge

Click to hear an explanation of the graph
Treatment
- Consider that there is no treatment because the
cells are harbored intracellularly and the titers decrease with
time.
- Ovariohsyterectomy or castration are the best
control methods as they remove the steroids that enhance organism
life.
Drugs
- Ampicillin (10 mg/kg TID 3 weeks) or LA 200 (20
mg/kg weekly 4 weeks) or Tetracycline (20 mg/kg TID 3 weeks)
followed by Strep. (20 mg/kg TID 3 weeks)
- Minocycline (25 mg/kg BID 2 weeks and Strep. (20
mg/kg BID 2 weeks), but this is very expensive !!!
- Nicoletti recommends tetracycline (20 mg/kg, q 8
hr, PO, 4 wks), gentamicin (1.5 mg/kg, q 8 hr, SC, 1 wk; or 2.5-3.0
mg/kg, BID). Dogs have successfully reproduced after this treatment.
- Treatment during pregnancy decreases chance of
abortion.
- 'Cures' should be suspect as the bug is
intracellular and titers decrease with time. The drugs may lead to a
transient abacteremia and fall in titer which is interpreted as a
'cure'.
- The flourinated quinilones offer hope for a
treatment.
- I would never treat a male because there is too
much chance that he could still spread the disease to a bitch.
Prevention
- B. canis testing every 6 months and before each
breeding. Have two negative tests 1 month apart prior to
introduction of a new dog.
- Have proper kennel hygiene. Use quaternary ammonium
and iodophor disinfectants. The organism is more hardy than some
Brucella.
- Eliminate all infected dogs. Keeping positive dogs
in a kennel because they are needed to produce puppies only
decreases the net number of puppies compared to if they were
eliminated.
- Kennels may be safe after 3 negative tests of all
dogs.
Public health
- The zoonotic potential is a concern, but not an
alarm. There have been 30 cases reported, and mostly in kennel
people with very few in pet owners.
|
 Next
Page
Next
Page Canine
Index
Canine
Index Next
Page
Next
Page Canine
Index
Canine
Index