|
Male
Reproductive Physiology
THERIOGENOLOGY OF THE
MALE
Functional anatomy Testes
-
Technically outside of peritoneum it is in an
outfolding of two layers
-
Visceral layer of
peritoneum fixed to tunica albuginea
-
Lumen of vaginal
process is continuous with peritoneal cavity
-
Parietal
layer of peritoneum fixed to scrotum
-
Shrinking
gubernaculum becomes proper ligament of testis joining caudal pole of testis to
tail of epididymis
-
Mediastinum testes: cord of
connective tissue running through testis
-
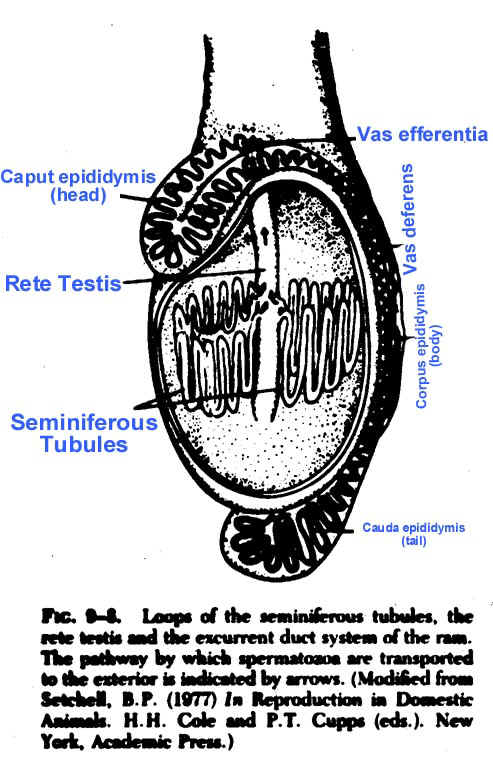
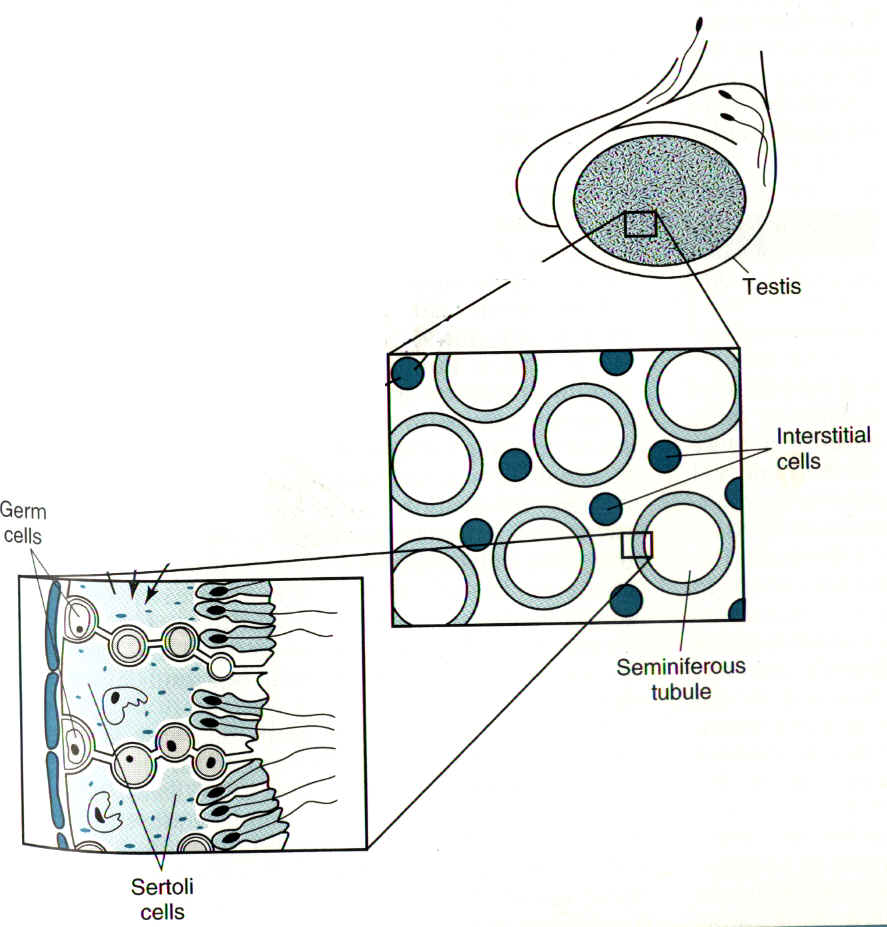
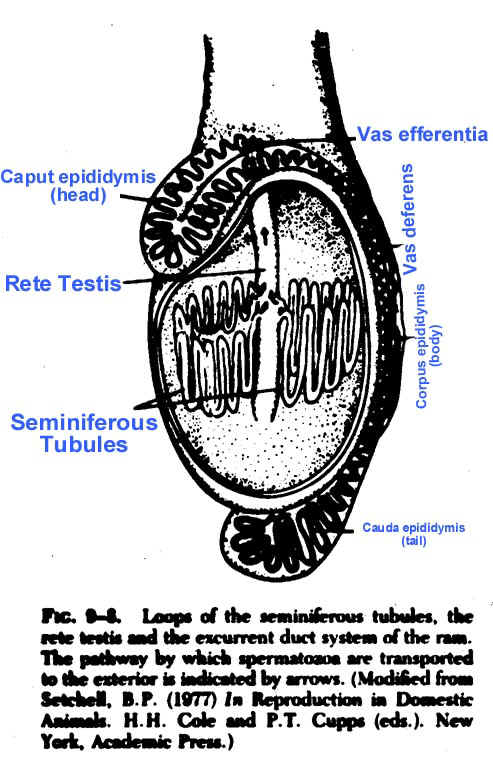
Seminiferous
tubules loop through the testis and connect to the rete testis
-
Rete
testis - collect sperm cells in center of testis
- androgen
binding protein (ABP)
- inhibin
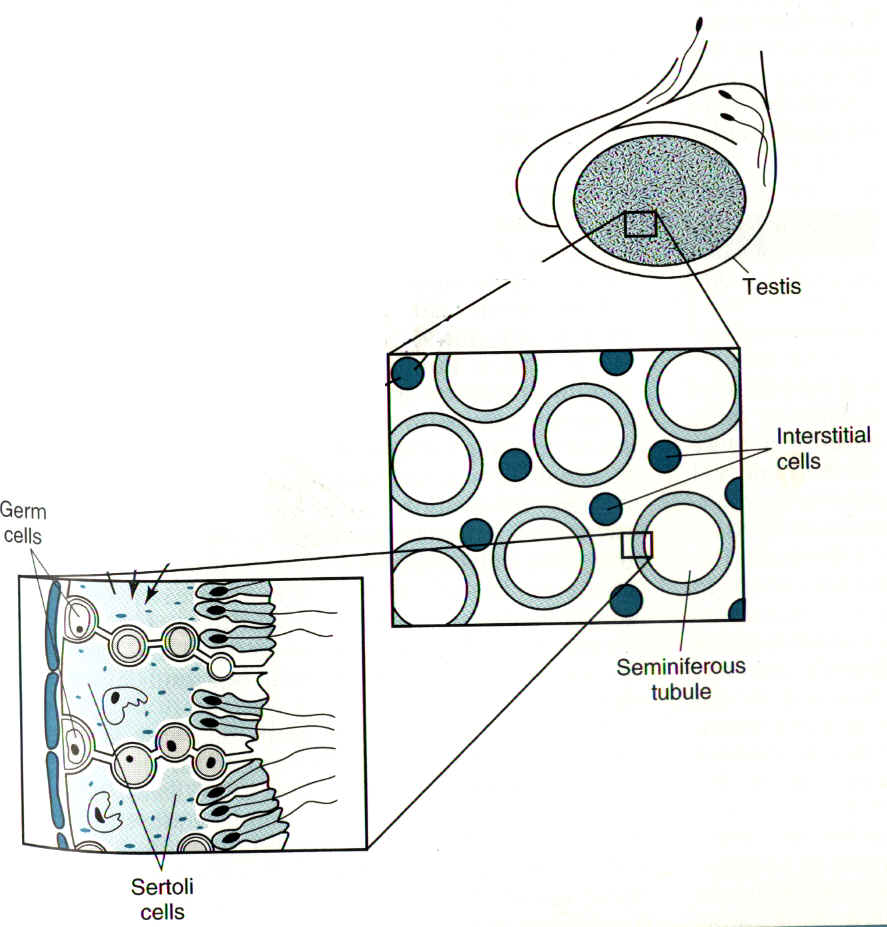
- Leydig
cells - interstitial cells
- Lie between seminiferous
tubules
- Secrete testosterone in response to LH
- Testoserone is pulsatile (chronic LH makes
testis refractory)
- Basement membrane - forms part of blood testis
barrier
- Myoid cells - forms part of blood testis barrier
- Tunica
albuginea
- Tough fibrous layer that forms capsule
- Sends projections down to the mediastinum
- Actually contracts to help 'pump' sperm cells
through rete
- Tunica vaginalis - peritoneal layer
Epididymis
- Caput
(head)
- Corpus (body)
- Cauda
(tail)
Human
testis above
Scrotum
- Skin
- Sweat glands
- Tunica
dartos
- Tunica parietalis
- Cavity
of vaginal process
- Hydrocele vs Hematocele
- Why a scrotum?
- Temperature regulation
- Sperm production does not occur normally at body
temperature
- Sweat gland cool
- Tunica Dartos contracts or relaxes to control the
closeness of the testis to the body
- Nerves are very sensitive to temperature changes
Spermatic cord
- From the inguinal ring to the testis
- Consists of the
- Ductus Deferens - enters urethra at colliculus seminalis
- Testicular artery
- Lymphatics
- Cremaster muscle
- Striated muscle from internal abdominal oblique
- Can only sustain short periods of contractions
(does not work well to pull up testis)
- Primarily a pumping action on the pampiniform
- Pampiniform plexus
- Spermatic artery and vein
- Artery and vein intertwined
- Form countercurrent exchange system
- Decreases temperature of blood
- Decreased pulse pressure - function not
known
- Testosterone contercurrent exchange also
|
Endocrine control of spermiogenesis
FSH interacts with Sertoli cells to cause:
-
Production of ABP (Androgen Binding Protein)
-
Conversion of testosterone to dihydrotestosterone and
estrogen
-
Stimulation of spermatocytogenesis
-
Completion of sperm release
-
Secretion of inhibin, which has a negative feedback
action on FSH release, GnRH
LH
- Results in hypertrophy of Leydig cells
- Stimulates production of testosterone by Leydigs
Androgens
- Major action is on Sertoli cell
- Produced by Leydig
- Diffuses into Sertoli and is secreted into blood - has
effects on brain, muscle, etc.
- Causes negative feedback at hypothalamus and pituitary
which inhibits LH release
- If administer exogenous testosterone, increased
systemic conc. will result in negative feedback, reducing LH and reducing
endogenous testosterone production, thereby inhibiting spermatogenesis
- If administer LH (or hCG) or GnRH, stimulate endogenous
testosterone production and don't upset balance of androgen within
tubule:androgen outside
- Relatively high level of testosterone (compared to
systemic circulation) required for spermatid migration
ABP
- Role is not to concentrate testosterone in tubule
- Most likely role is to transport testosterone to head
of epididymis
Inhibin
- From Sertoli cell
- Paracrine, autocrine and endocrine action
- Negative action on FSH, GnRH
Estrogen
- Produced in Sertoli cells by conersion of testosterone
- Paracrine, autocrine and endocrine action
- Negative action on FSH
- Positive action on LH
|
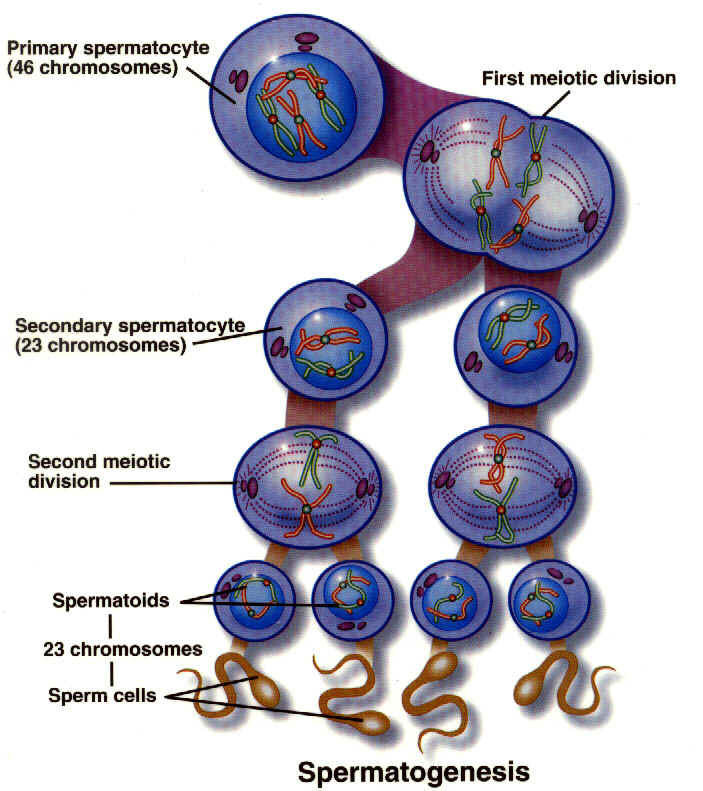
Spermatogenesis
Spermatogenesis
(Entire process from spermatogonia to spermatozoa)
|
Spermatogenesis
|
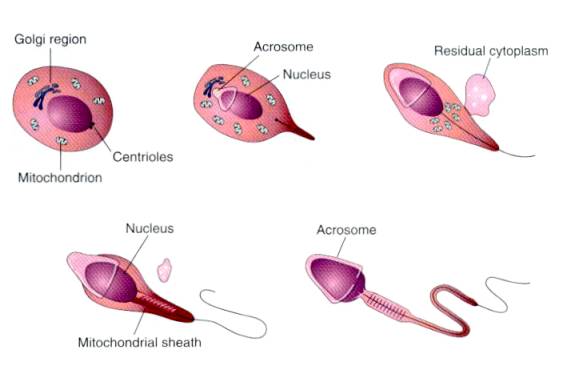
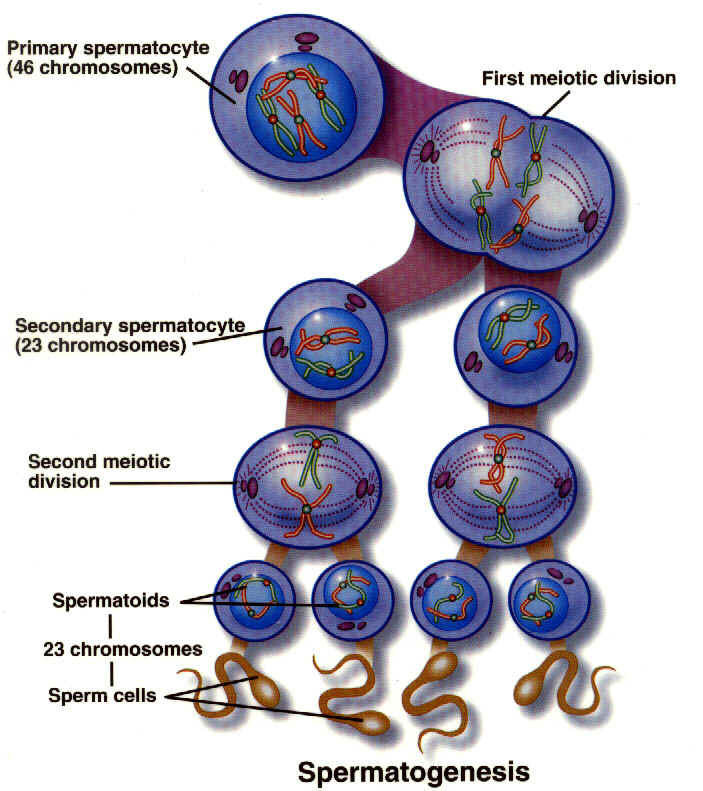
- Mitosis of spermatogonia and meiosis with
differentiation into sperm takes 5-7 weeks in most mammals
- Renewal of stem cells
- Five mitotic divisions produce 16 primary spermatocytes
- Two meiotic divisions produce 64 spermatids
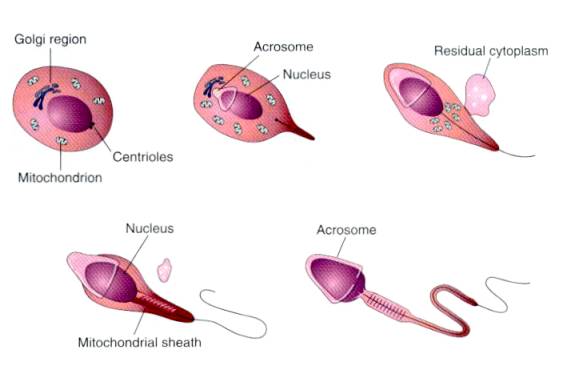
- Spermiogenesis (spermateliosis)
- Spermatids differentiate from compact spherical cell
into spermatozoa without cell division
- Golgi granules coalesce to form acrosome
- One centriole gives rise to flagellum, other gives rise
to basal plate
- Nucleus moves to periphery and chromatin condenses
- Spermatid rotates so tail sticks out into lumen
- Mitochondria congregate around flagellum and become
localized in midpiece
- Most of cytoplasmic mass is engulfed by Sertoli cells
when spermatozoa are released into lumen of seminiferous tubule, small
amount remains at neck (proximal cytoplasmic droplet)
- Proximal droplet moves to distal end of midpiece during
epididymal passage
- Distal droplet is lost during storage in the epididymis
or during ejaculation
|
|
Sperm cell
- First described approx. 300 yrs ago
- Realized essential for fertilization around 1830
- Covered by plasma membrane
- Acrosome contains hydrolytic enxzymes (acrosin,
hyaluronidase, etc.)
- Postacrosomal region is where attachment and fusion to
oolemma takes place
- Tail Responsible for motility
- Midpiece (mitochondria)
- Principle piece
- End piece
- 9:2 arrangement of doublets
- Kartagener's syndrome - lack 9:2 arrangement; immotile
cilia syndrome (infertility,respiratory infections, situs inversus)
|
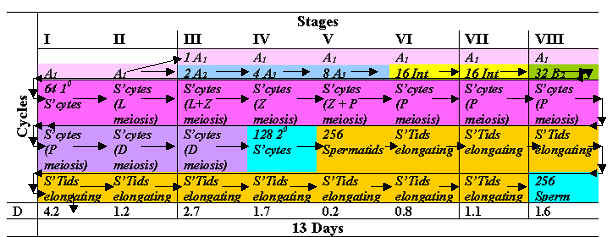
Spermatogenic cycle (time)
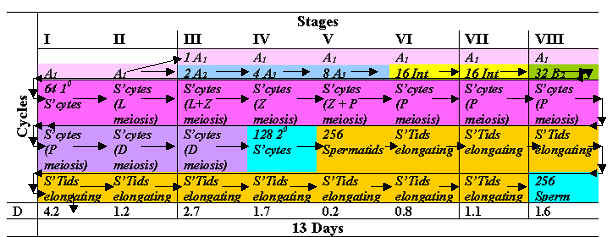
- Changes with time in the appearance of one section of a
tubule; series of changes in a given area of seminiferous epithelium
- Based on cell associations of different stages of
spermatogonia, spermatocyte, spermatid, spermatozoa within one section of a
seminiferous tubule
- In any given area of a tubule, stem cells initiate
series of mitotic divisions preceding meiosis at extremely regular intervals
- Time from spermatogonium to spermatozoa is remarkably
constant, cannot speed up process
- Each step of spermatogenesis has a fixed and constant
duration
- Before spermatozoa are fully formed as a result of one
cycle, three new cycles have started, four different stages of cells are
associated with each other in one section of tubule at any one time
Spermatogenic wave (space)
- Sequential change in stage of cycle along the length of
the tubule
- In each sequential segment of tubule, a sequential
stage of the cycle is found
Blood testis barrier
- Primary component is tight junctions between Sertoli
cells which divide tubules into 2 compartments
- Basal compartment - contains spermatogonium and
preleptotene spermatocytes (2n)
- Adluminal compartment - communicates with lumen of
tubule and contains more advanced stages (1n)
- Demonstrates wide range of permeability from complete
exclusion of some substances to nearly free transfer of others
- Not only excludes some substances (such as antibodies)
but functions in retaining others (such as Androgen Binding Protein, inhibin)
- Functions in keeping haploid cells from initiating
immune reaction
- Incomplete or partial barrier of myoid cells
surrounding tubule also a component
- Fluid
- Sertoli cells secrete fluid which transports immotile
sperm from tubules
- Rete apparently secretes fluid also (although some
claim evidence is lacking)
- Sperm movement is by fluid secretion, cilia movement
and contractile elements (myoid layer)
Sperm Maturation
Epididymis
- Maturation and storage of sperm
- Head
- Not motile - swim in circular motion
- Not fertile
- Proximal droplet
- Low disulfide linkage
- Fluid absortion
- Body
- First see some forward motility in body
- Some fertility
- Droplet moving down
- More disulfide linkage
- Binds oocytes
- Tail
- Normal motility
- Fertile
- Distal droplet
- Hiigh disulfide linkage
- Binds oocytes
- Transport takes 9-13 d depending on species - mandatory
Sperm Delivery
Accessory glands
- Contributions not needed for fertility
- Coating of gland secretion removed during capacitaion
- Ampulla
-
- thickened glandular portion of ductus deferens as it connects with urethra
- Large in stallion, bull
- Present in
dog but not always grossly visible
- Absent in boar, tom
-
Vesicular glands (seminal vesicles) - sac like organs with
lobulated surface
- Provide volume, protein, sugars,
salts
- Generally fill before copulation and empty
during ejaculation
- Boar - store large volume of fluid
-
Bull - more a solid mass of tissue, produces only small
volume of fluid
- Absent in tom, dog
- Stallion
- fills during sexual stimulation
- Prostate - solid
tissue mass which secretes during copulation
- Animals
with extended copulation times (boar and dog) have high volume contribution from
prostate
- Secretion mainly ionic compounds (NaCl, Na
citrate, and variety of enzymes)
- Present in all
domestic species
- Bull and boar - anterior mass is body
of prostate, disseminated portion is pars disseminata
- Bulbourethral
(Cowper's) - small, except in boar; muscular gland associated with caudal pelvic
urethra
- Boar - large gland containing large volume of
stored gel (sialic acid) which is emitted during ejaculation
- Can
differentiate castrated from cryptorchid pig on basis of rectal palpation.
In ruminant and boar, ducts open into urethral recess,
situated dorsally, which may prevent passage of catheter
|
| |
Bull |
Stallion |
Boar |
Dog |
Cat |
| Ampullae |
+ |
+ |
_ |
+? |
_ |
| Seminal vesicle |
+ |
+ |
+ |
_ |
_ |
| Prostate |
+ |
+ |
+ |
+ |
+ |
| Bulbourethral gland |
+ |
+ |
++ |
_ |
+ |
Penis
Penis
- Root -right
and left crura, crus penis
- Corpus (body)
- Shaft
-
Glans penis ornamental tip, may refer to portion of penis
distal to attachment of free prepuce
- Richly supplied
with sensory nerves which respond to heat and moisture; normal sensation
necessary to locate vagina, make intromission and initiate ejaculation
- Corpus
cavernosum penis
- Arises as pair of crura under
ischiocavernosus m.
- Continues to tip as paired
cavernous body
- Corpus spongiosum penis - surrounds
urethra
- Enlarged at ischial arch to form penile bulb
which is covered by striated bulbospongiosum m.
- Corpus
spongiosum glandis - erectile body of glans
- Tunica
albuginea
- thick fibroblastic covering of the cavernous bodies,
- capable of
withstanding very high internal pressures
- Species
differences
- Fibroelastic -
- small
volume, minimal increase in size -
- thick tunica albuginea,
- trabeculae contain
large amount of supporting tissue with small cavernous spaces
- high
pressure sigmoid flexure straightens to elongate
in bull, ram, buck
- temperature
sensitive vaginal ejaculation
- raphe
penis (surgical landmark)
- preputial frenulum -
- remnant
of developmental attachment apical ligament - fibrous
band, originates on tunica albuginea proximal to fornix, extends to level of
glans where it inserts on tunica albuginea;
- supports penis during erection;
- if a
bull becomes "hyper-erect" the apical ligament will pull the tip back
into a spiral; this is considered normal after intromission but is a problem if
it occurs before intromission
- buck, ram have long
urethral process boar corkscrew
tip preputial diverticulum pressure
sensitive cervical ejaculation
- Vascular
penis
- low pressure high
volume -
- large cavernous spaces,
- little supporting tissue,
- large increase in
size stallion
- "bell"
- glans swells during ejaculation
- urethral process,
-
urethral fossa,
- fossa glandis
- urethral sinus -
- dorsal
diverticulum,
- bean - smegma
- pressure and temp
sensitive
- fractions
- pre -
bulbourethral
- sperm rich - ampullary
- post
- seminal vesicles
- Vascular penis with os penis
-
Dog os penis (baculum) - extends
from tip to bulbus glandis
-
Bulbus glandis - proximal
portion of penis - swells to 2-3 times the diameter of the shaft during
copulation
- Feline projects
posteriorly small os penis spines
on surface of penis
- Retractor penis muscles - control
length of penis in ruminants and swine by action on sigmoid flexure
- Ischiocavernosus
m. - important in causing erection, pumps blood into corpus cavernosum penis by
compressing dorsal vein against ischial arch
- Prepuce - Non-haired skin,
not mucous membrane
- Loosely arranged elastic layers
which allow penis to extend
- Sheath - externally
visible container for prepuce and penis
|
Erection
- Arteriole
expansion
- Venule contraction
- Relaxation of retractor
- Contraction of ischiovavernous muscle
- Filling of coprpus cavernosum
- Parasympahthetic
-
Emission - Sympathetic Movement
of sperm to pelvic urethra
-
Viagra (Sildenafil), Cialis (tadalafil)
 
- Erection
- The physiologic mechanism of erection of the penis involves release of
nitric oxide (NO) in the corpus cavernosum during sexual
stimulation.
- NO then activates the enzyme guanylate cyclase, which results in
increased levels of cyclic guanosine monophosphate (cGMP) producing
smooth muscle relaxation in the corpus cavernosum and allowing inflow of
blood.
- Sildenafil has no direct relaxant effect on isolated human corpus
cavernosum, but enhances the effect of nitric oxide (NO) by inhibiting
phosphodiesterase type 5 (PDE5)
- Responsible for degradation of cGMP in the corpus cavernosum.
- When sexual stimulation causes local release of NO, inhibition of PDE5 by
sildenafil causes increased levels of cGMP in the corpus cavernosum,
resulting in smooth muscle relaxation and inflow of blood to the corpus
cavernosum.
- Sildenafil at recommended doses has no effect in the absence of sexual
stimulation.
|
Male reproductive features of the
domestic species.
| |
Bull |
Stallion |
Boar |
Dog |
Cat |
| Testis orientation |
cauda down |
horizontal |
perineal, cauda up |
horizontal |
perineal, cauda up |
| Ampullae |
+ |
+ |
_ |
+? |
_ |
| Seminal vesicle |
+ |
+ |
+ |
_ |
_ |
| Prostate |
+ |
+ |
+ |
+ |
+ |
| Bulbourethral gland |
+ |
+ |
++ |
_ |
+ |
| Penis type |
fibroelastic |
vascular |
fibroelastic |
vascular, os |
vascular, os |
| Copulation duration |
1 second |
20 sec |
6 min |
20 min |
seconds |
| Volume (typical) |
5 cc |
60 cc |
200 cc |
20 cc |
0.04 cc |
| Sperm conc. |
1.2 |
.10 |
.15 |
NA |
1.7 |
| Total cells in ejaculate |
6 |
6 |
30 |
.5 |
0.057 |
| Site of semen deposition in
female |
vagina |
cervix / uterus |
cervix |
vagina |
vagina |
This stuff is just being held here now, I will
move it.
Male sexual development
- Migration of primordial germ cells to gonadal ridge
- In presence of Y chromosome - formation of primary sex
cords which become germinal epithelium of seminifreous tubules; in absence -
cells form into medullary pattern
- Rete testis establishes connection between mesonephric
(Wolffian) tubules and seminiferous tubules; mesonephric tubules form
efferent ductules in head of epididymis and mesonephric duct forms rest of
epididymis, ductus deferens and seminal vesicles
- Fetal androgen causes development of male reproductive
tract
- Müllerian inhibiting substance suppresses development
of paramesonephric (Müllerian) ducts
- Formation of vaginal process (a peritoneal sac
extending through abdominal wall) - encloses inguinal ligament of testis
which, along with diaphragmatic ligament together with mesorchium suspends
fetal testes, inguinal ligament connects testis and mesonephric duct, distal
to this it is called the gubernaculum testis and terminates in the region of
the scrotal rudiments
- Descent of testes
- Secretion of "descendin" from normal testes
results in selective growth of gubernaculum
- Gubernaculum outgrowth results in masculinization of
inguinal canal
- Intraabdominal pressure transmitted to gubernaculum
which in turn applies traction to testes to introduce it into ing. canal
- Descent of testis into and through ing. canal is
interplay between intra-abdominal pressure transmitted by patent processus
vaginalis and androgen induced gubernacular regression
- Androgens, under the control of intact fetal
hypothalamic-pituitary axis, alter visco-elastic properties of gubernaculum;
reductions in turgidity of gubernaculum allow intra-abdom. pressure to push
testes into scrotum
- Intact hypoth-pit axis necessary for testicular descent
- Alterations in maternal-placental-gonadal axis may be
responsible for abnormal male phenotype
- descendin stimulates, estrogen inhibits gubernac.
growth
- Consequences of failure of descent
- Cryptorchid - unilateral or bilateral
- bilateral - normal sexual phenotype, libido, androgens,
but sterile due to relatively high intraabdominal temp.
- may not be sterile if testes in inguinal canal
- Mechanisms to maintain lower temp in testes
- dartos muscle in scrotum
- inc/dec surface area
- inc/dec thickness of skin
- cremaster muscle in spermatic cord - raises or lowers
testes
- pampiniform plexus - countercurrent mechanism
- temperature receptors in scrotal skin can elicit
responses that tend to lower whole body temp (sweating, panting)
Genetic sex
- Determined at time of fertilization
- Presence of testis determining factor (TDF) of Y
chromosome causes mesonephros to form sex cords; in absence of Y chromosome
cells form into a medullary pattern
- H-Y antigen, once thought to be TDF is now considered a
minor histocompatibility antigen in close proximity to the TDF
Hormonal sex
- Hormones produced by gonad depend on what gonad
resembles, regardless of chromosomes
- Fetal testis grafted against ovary of female fetus -get
Müllerian inhibition and Wolffian development on that side only (local
effect)
- If use testosterone implant -get Müllerian and Wolffian
development, lack Mullerian Inhibiting Factor from testis
Abnormal sexual development (some examples)
Hermaphrodite - possess both ovaries and testes
Pseudohermaphrodite - possess only one type
gonad, named for gonad
- Female pseudohemaphrodite (male phenotype with ovaries)
- Inherited in Cockers, German Shorthair, Pug, Kerry
Blue, Weimaraner
- TdY transposes to autosome
- Simple autosomal recessive
- AA, AY develop normally
- AA* and A*Y develop normally but are carriers
- A*A* are affected, look like males
- affected animals are HY antigen positive
- usually have ovotestes or ovaries and ovotestes; rarely
have testes and ovotestes
- phenotype depends on amount of testicular tissue
- possess Mullerian ducts (MIF receptors present, timing
problem?)
- XX sex reversal (mice, goats, pigs, dogs)
- Autosomal dominant gene (Sxr) acts like a Y chromosome
- Goats: autosomal gene with Y effect is on chromosome
which controls polledness.
- Intersex and hornedness are recessive.
- Polled
gene is dominant.
- Sexual differentiation of heterozygous polled goat is
unaffected but homozygous are hermaphrodites.
- Most polled intersex goats are
male pseudohermaphrodites and genotypically female (XX).
- Homozygous bucks
tend to become sterile due to a blockage in the head of the epididymis, in
older bucks the seminiferous tubules close to the rete testis degenerate or
rupture leading to the formation of sperm granulomas
- Dogs: American Cocker Spaniel -autosomal recessive, XX
males and XX true hermaphrodites have been described
- XY sex reversal (horses):
- autosomal, sex-linked
dominant gene or Y chromosome mutation,
- affected individuals range from
phenotypically normal but sterile mares with inactive ovaries and normal
tubular genitalia to individuals with streak gonads or ovotestes and
hypoplastic or aplastic tubular genitalia
- Androgen insensitivity - Testicular feminization
(humans, mice, rats, cats, cattle, horses):
- XY genotype,
- possess
testosterone producing testes but neither Müllerian or Mullerian duct
systems;
- external genitalia female,
- deficiency of intracellular androgen
receptors,
- sensitivity to MIF is retained and MIF is produced;
- horses are
unique in that they retain male behavior patterns
- Persistent Müllerian duct syndrome (dogs):
- XY males with testes and normal masculinization of
internal and external genitalia but possess complete tubular female tract;
- Autosomal recessive
- thought to be due to receptor defect
- Min. Schnauzer, Basset, cat
- Freemarttin
- Heifer born twin to a bull
- 11/12 sterile
- Chimera of XX/XY from placental anastamoses
- XY prevents uterine development
- Males also have dec. fertility
- XO
- Fetal ovaries form but XO oocytes undergo rapid atresia
- No germ cells at birth
- No estrogen
- Humans - short, infertile; normal genitalia
- Mares - documented but rare
- XXX, XXY - survive by inactivating X
Tortoise shell cat
- B = black (dominant), b = yellow (recessive), on X
chromosome
- XB XB = black; XbXb = yellow; XB Xb = tortoise shell
- Male tortoise shell
- XB XbY - sterile
- XB Xb / XY chimera
- fertile
- most are of this type
contributed by Bruce
E Eilts and modified on 1
November 2004
assisted by Emma Jones Eric Huey
|