Problems
of Bovine Pregnancy

303-305,
400-401
Elective termination of pregnancy:
- The indications for elective termination of pregnancy include:
- Inadvertent breeding, such as breeding to the wrong bull, a heifer
that was too small when bred, and feedlot heifers;
- Pathologic
pregnancies such as hydrallantois.
- It should be remembered when
trying to abort feedlot heifers that if they are receiving a
progestin type growth promotant that administration should be
stopped while trying to abort them to prevent the CL
"rescue" phenomenon.
- Physical methods to terminate pregnancy include rupture of
amniotic vesicle before 65 d of gestation.
- The fetal membranes may
remain in utero for 2-3 wks after AV rupture.
- Decapitation of fetus
may be performed, usually between 65 to 90 days. It becomes
difficult after 3 mo.
- Abortion will occur in 10-14 d, the fetus may
mummify.
- Intrauterine infusions can result in pregnancy loss.
-
Enucleation of CL, although practiced in the past, is NOT
RECOMMENDED. It may result in hemorrhage (sometimes fatal) and
adhesions. It was used before PGF became available.
- Hormonal methods of
pregnancy termination
- More common than physical methods.
- During normal pregnancy, the CL is required
for the first 5 month and the last month of gestation. An extra-gonadal
source (placenta) (plus adrenals?) is available during the remainder
of gestation.
- To terminate pregnancy during the first 5 mo use PGF,
during the 6th, 7th and 8th month use PGF plus a corticosteroid
(usually dexamethasone).
- If PGF is used alone, there is sometimes
incomplete luteolysis and placental progesterone production may
rescue the pregnancy.
- Corticosteroid alone although it reduces
placental secretion of progesterone, does not cause luteolysis until
the last month of gestation. The fetoplacental unit must be mature
in order for corticosteroids to terminate pregnancy.
- During the last
month, either PGF or corticosteroid is usually sufficient.
- Estrogens
were used before PGF was available but in general have poor
efficacy. Estrogens are more reliable in the first 5 months, but PGF is
more so.
Induction of parturition:
- There are a number of indications for induction of parturition.
These include:
- 1)health of the cow - either to save her or to save
the calf because of the dam's deteriorating condition;
- 2)prevent
dystocia? - induction of parturition has been proposed as a means of
reducing dystocia because the calf gains up to 1.0 kg/d near the end
of gestation;
- 3)in dairy cattle parturition may be induced to
prevent excessive udder edema from damaging the udder supports;
- 4)in
beef cattle induction of parturition can be used to truncate the
calving season, thereby allowing more time postpartum to resume
cyclicity before the next breeding season;
- 5)management
considerations, e.g. more efficient use of facilities and manpower;
-
6)seasonal calving to allow better use of available feeds (more
common in New Zealand);
- 7)allow closer supervision to be able to
provide assistance at the earliest indication (especially with
valuable animals such as embryo transfer calves).
- There are important criteria to be met for a method to be
considered successful. A method should:
- 1)be efficacious,
- 2)provide
a predictable time of delivery,
- 3)have no adverse effects on the
health of the dam,
- 4)have no adverse effects on the health of the
offspring,
- 5)alter neither the quantity nor quality of colostrum,
-
6)not affect postpartum involution or subsequent fertility,
- 7)not
increase the incidence of retained placenta.
- Some precautions should
be considered for a successful outcome.
- You should have a fairly
accurate and reliable breeding date because while calves born up to
2 wks early have normal vigor, those born more than 2 wks premature
have reduced viability.
- If a large number of animals is to be
induced, consider the needs of a large number of calves and
husbandry requirements.
Methods used to induce parturition in cattle:
- Long acting corticosteroids are insoluble esters or
suspensions such as:
- Dexamethasone trimethylacetate (20 mg),
-
Triamcinolone acetonide (10 mg),
- Flumethasone suspension (10 mg),
-
Betamethasone suspension (20 mg).
- These are injected i.m.,
approximately 1 mo. prior to the due date.
- Parturition occurs in
4-26 d. This wide range is a disadvantage in some respects.
-
Preexisting health conditions in the dam may be exacerbated because
of the long acting corticosteroids.
- The incidence of retained fetal
membranes is low (9-22%) compared to other methods of induction.
- However, there is a high incidence of calf mortality (17-45%).
- Calf
mortality is due to premature placental separation and uterine
inertia.
- The calves die in utero and are born partially autolysed
with the membranes intact.
- Hypogammaglobulinemia is frequent in
calves born alive. This is because colostral immunoglobulins are
reduced and in addition the calves are often weak and ingest
inadequate amounts of colostrum.
- Short acting corticosteroids are soluble esters such as:
-
Dexamethasone (20-30 mg),
- Flumethasone (8-10 mg),
- Betamethasone
(30 mg).
- They are generally efficacious (80-100%).
- They can be
injected i.m. within 2 wks of the due date.
- Parturition usually
occurs in 24 to 72 h, with an average of 48 h.
- There is no increase
in calf mortality if used within 2 wks of term. Earlier than this
there is the risk of inducing a premature calf.
- Colostral
immunoglobulins are normal.
- The major disadvantage is an increased
incidence of retained fetal membranes.
- The likelihood of retained
fetal membranes is related to the degree of prematurity and ranges
from 30 to 100%.
- The earlier parturition is induced, the higher the
percent of retained fetal membranes.
Prostaglandins :
- Drugs available at this time in the US include:
- Prostaglandin F2a
(25 mg),
- Cloprostenol ( 500 ug),
- Fenprostalene (1 mg).
- They are
similar to short acting corticosteroids as far as efficacy, time
from administration to expected calving, incidence of retained
placentas, etc.
- They have no great advantage over corticosteroids.
Estrogens:
- These are generally considered an "old" method, used
before prostaglandins were available. They have relatively poor
efficacy (60-80%). They also have a high incidence of retained
placentas.
- Combinations:
- Combining short acting corticosteroids and estrogens does not
decrease the incidence of retained fetal membranes. Large doses of
estrogens decreases the interval to parturition by several hours and
reduces induction failures.
- If long acting corticosteroids are followed by short acting
corticosteroids or prostaglandins 7-12 d later, most cows will calve
2-3 d after the second injection. The interval is shorter and more
predictable with PGF, however, the incidence of calf mortality is
still high.
- Using a combination of corticosteroid plus prostaglandin does not
decrease the percent of retained fetal membranes. However, there are
fewer induction failures, but there is no real advantage.
Problems of pregnancy
Dropsy conditions include hydrallantois and hydramnios.
- Hydroallantois, or hydrops of the allantois, is due to a
defective placenta (the chorio-allantois).
- The fetus is normal.
- The
condition is characterized by a rapid accumulation of watery,
clear fluid, usually in the last trimester.
- The cow is rounded in
the caudal view, and you normally can't palpate the fetus or
placentomes.

- Usually the condition results in a sick cow with
anorexia, decreased rumen motility, dehydration and weakness.
- The
cow may be down.
- The placenta is thick.
- If the cow survives,
postpartum metritis is common.
- The condition usually ends in death
or intervention.
- The prognosis is guarded to poor for life and
fertility.
- Treatment consists of Caesarian section with a slow
drainage of fluid and perioperative support.
- Dexamethasone can be
used if the cow is not down.

- Hydramnios, or hydrops amnios, is due to a defective calf,
usually attributed at least partly to a defect in swallowing.
- The
placenta is normal.
- The condition is characterized by a gradual
accumulation of thick, viscid fluid during the last half of
gestation.
- The cow has a pear shaped caudal view.
- Usually you can
palpate the fetus and placentomes.
- The cow is clinically
otherwise unaffected.
- The pregnancy usually goes to term, and
frequently a small, deformed fetus is delivered.
- Postpartum metritis
is uncommon.
- The prognosis is good for life and fertility.
- No
treatment is required.
- The cow may be allowed to go to term or
induced to calve.
Uterine torsion
- Uterine torsion usually occurs near term and is usually found at
parturition because of the subsequent dystocia.
- The attachments of
uterus and manner in which cows rise are assumed to play a role in
the development of this condition.
- Diagnosis can be made by a number
of ways.
- By manual vaginal exam, the vaginal wall can be felt to be
twisted or spiraled. This can be visualized with the aid of a
speculum.
- By rectal exam, the broad ligaments can be felt to be
crossed and the uterus twisted. The vulva can often be seen to have
a slight twist of the dorsal portion.
- It is important to determine
the direction of the torsion during the examination.
- When correcting
a dystocia, if the calf is found upside down (dorso-pubic), consider
the possibility of a uterine torsion.
- Before and during correction,
insure that things are going in the proper direction.
- If the cervix
is open, a detorsion rod may be used.
- Alternatively, the torsion may
be corrected manually by rocking the fetus until enough momentum is
achieved to flip the uterus.
- If the cervix is closed other methods
must be employed such as the "Plank in flank" method or
surgical (C-section) correction.
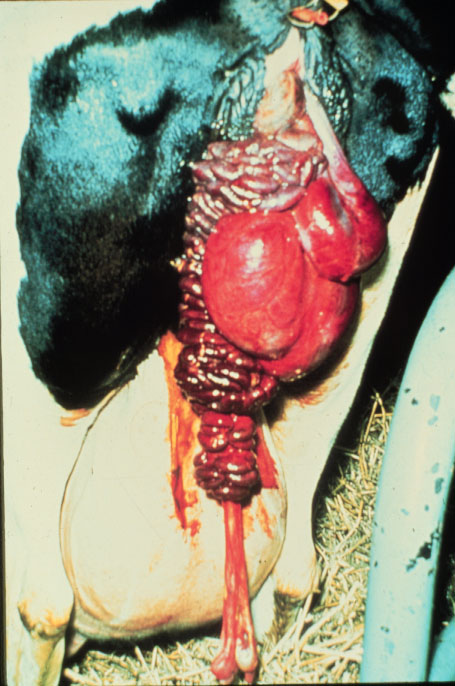
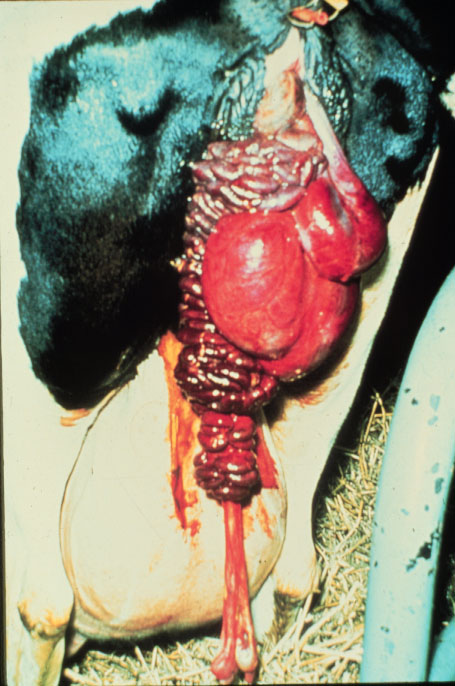
Uterine Prolapse
- Lay terms for this condition include "cast her wethers"
and "lost her calf bed". This is a true emergency.
This is an acute condition that is often associated with
hypocalcemia and may also follow use of great force in fetal
extraction. It is not hereditary.
- Diagnosis is fairly obvious, caruncles can be observed on the
uterus which is prolapsed through the vulva. The prolapse can
involve other organs such as the bladder or intestines. In some
cases, the uterine artery may rupture with fatal consequences.

- The prognosis is relatively good if the uterus does not suffer too
much trauma and is replaced properly. The chance of recurrence not
great. If properly corrected, there are no serious long term
effects, although there may be a slight increase in days open during
that lactation.
- Correction is accomplished by first cleaning
the uterus to remove dirt and accumulated debris.
- Proper restraint
is essential.
- Epidural anesthesia is helpful to prevent straining.
-
To aid in replacing the uterus, tip the pelvis cranially by placing
the cow in a "frog leg" position and elevate the uterus
(either by elevating the hind quarters of the cow or having
assistants hold the uterus up).
- It may help to empty the bladder if
it is trapped.
- Generally the placenta is removed only if loose.
- More
trauma is caused to the endometrium by manually removing the
placenta than by leaving some attached to the uterus.
- Sugar or other
such substances are sometimes used in an attempt to reduce the edema
in the uterus and shrink it down. However, the effect is not
remarkable.
- Oxytetracycline powder or other broad spectrum
antibiotics are sprinkled on the uterus before replacement or placed
in the uterus after replacement.
- Complete replacement is
essential to prevent continued straining and reoccurrence.
- Some
recommend suturing the vulva after replacement with heavy suture
material in something like a large horizontal pattern. Although this
is often done, it is considered a placebo procedure if the uterus
has been properly replaced.
- Oxytocin should be given after
replacement. If given before replacement, the uterus will contract
down and make the job more difficult.
- It is important to treat milk
fever first before replacement because that is a more life
threatening condition.
- Hysterectomy is considered a salvage
procedure.

Vaginal prolapse
- This is often a chronic condition and is hereditary.
- There is a
breed predisposition with Hereford, Santa Gertrudis being
predisposed.
- Vaginal prolapses often recur. For this reason, it is
recommended to cull cattle with a vaginal prolapse.
- They usually
occur prepartum, in late gestation, when the cow is under the
influence of rising estrogen and experiencing relaxation of the
tissues.
- They may occur postpartum or may be associated with
follicular cysts.
- Upon presentation, the vagina, with or without the
cervix, is seen protruding from the vulva.

- The tissue is often dry
and necrotic.
- Tenesmus is common.
- When considering the prognosis,
although rarely life threatening, consider the chance of recurrence
and inheritance and recommend culling.
- These are much easier to
replace but harder to maintain in the correct position.
- Correction is aided and tenesmus reduced with an epidural.
- The
tissue is cleaned,, lubricated and replaced.
- After replacing the
prolapse, the cow may be maintained so that her hind quarters are
elevated (dairy cow)
- These need to be sutured to help reduce the
risk of reoccurrence.
- There are numerous methods of fixation.
- Probably one of the most effective is the Bühner stitch.
- This
requires a Bühner needle and Bühner tape. If other material
such as umbilical tape is used, results are unsatisfactory.
Umbilical tape, for example, will break and also wicks bacteria.

- The Bühner stitch must be removed prior to parturition.
- Minchev's
technique is useful prepartum, especially in cattle that cannot be
watched closely because they are able to calve with the Minchev
buttons in place.

- Tissue trauma, swelling and inflammation may be a
problem.
- Other techniques commonly used include:
- The
"boot-lace", where eyelets are made from hog rings or
sutures. This can be removed temporarily and replaced by lay help,
for example in prepartum cases.

- Modified Caslick's are also used occasionally with varying degrees of
success.
- Pessaries are also used occasionally with varying degrees of
success.
- Trusses, etc. are also used occasionally with varying degrees of
success.
Fetal mummification
- This occurs in cases of fetal death without involution of the
corpus luteum and fetal expulsion, followed by autolytic changes,
absorption of the fetal fluids and involution of the placenta.
- In
cows the maternal caruncle involutes and hemorrhage occurs between
the placenta and the endometrium, leaving a reddish-brown, gummy
mass that imparts a reddish brown color to the mummified fetus.
- The
etiology is varied and ranges from infectious causes such as BVD,
leptospirosis, etc. to non-infectious causes such as genetic,
compressed umbilical cord, etc.
- Diagnosis is based on the presence of a CL, the lack of fremitus
in the uterine artery and lack of fetal fluid in the uterus. The
fetus feels dry and mummy-like on palpation. Oftentimes the head,
ribs, etc. can be felt.
- Prognosis is good if the fetus is removed. After the fetus
is removed, conception usually occurs 1-3 mo. later.
- Treatment is accomplished by administering PGF2a (with or without
estrogen) to lyse the CL. Steroids are ineffective with dead fetus
and non-functioning placenta. After treatment, check the vagina
because sometimes the mummy may be lodged in the vagina when
expelled.


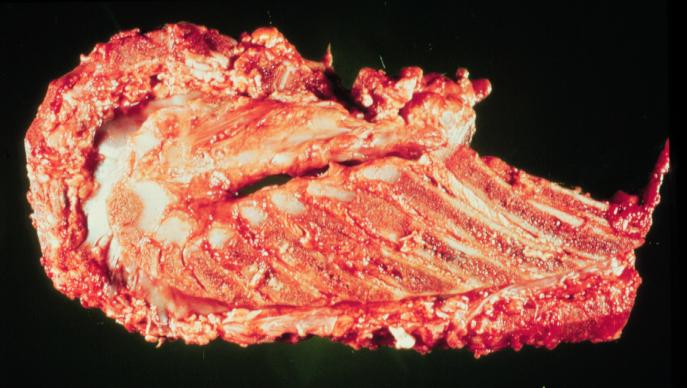
Fetal Maceration
- Fetal maceration results from death of the fetus followed by
dilation of the cervix and incomplete abortion or dystocia, usually
during the last half of gestation. This condition can be due to a
variety of miscellaneous organisms.
Diagnosis
- On palpation per rectum, the uterine wall is thick, little or no
fluid is present in the uterus and you may be able to palpate fetal
bones and pus, or bones crepitating against each other in the
uterus.


Prognosis
- The prognosis is poor for cows with this condition. This is not a
"retained CL" problem so lysis of the Cl is not helpful.
Endometrial damage is present even if all fetal parts are removed.
Treatment
- Treatment is very difficult. The cervix cannot usually be dilated
sufficiently to remove all the fetal parts and any remaining fetal
parts act as an IUD. Surgery has been performed in valuable
individuals but is very difficult.
Calving Injuries
- Postpartum hemorrhage: This can be due to a variety of
causes. When observed, the origin of the blood should first be
determined.
- Lacerations or tears are usually due to mishandling
during OB procedures.
- Tears in the uterus are usually located in dorsally, near
the cervix. They can be diagnosed by palpation or visually.
-
(Sideline: Schistosomus reflexus should be included in the
differential diagnosis when viscera are observed protruding from the
vulva or palpable during an obstetrical procedure.
- This is a
congenital defect where the spine is bent back on itself in a
hairpin turn and the ventral body wall is not closed.
- This defect is
incompatible with life although the calf may be alive at the time of
attempted delivery.
- Delivery requires a fetotomy or cesarian
section.)

- The prognosis in the case of lacerations of the reproductive
tract varies with the location and
extent of the tear.
- Peritonitis is a possible sequela.
- Small tears
may heal without treatment.
- Larger ones should be sutured, either
via laparotomy (difficult) or by intentionally prolapsing the
uterus. This can reportedly be achieved by administering 10 cc
epinephrine i.v., but is not effective after oxytocin
administration.
- Cervical tears can result in profuse bleeding. Not as
critical to future fertility as in the mare but may reduce fertility
depending on the extent. No real treatment, rather try to prevent.
- Vaginal tears are not uncommon. They may go unnoticed
unless they result in hemorrhage.
- There are large arteries at the
1:00-2:00 and 10:00-11:00 positions.
- Otherwise, a vaginal tear may
be noticed because of masses of fat protruding from the vulva after
calving or during a vaginal exam.
- During the postpartum period they
may be suspected during a rectal exam when hard masses are palpated
in the vaginal area.
- Again, the prognosis varies, depending on the
location and extent.
- If significant hemorrhage is occurring, place a
pair of hemostats on the artery for 24 h.
- Attempting to suture the
artery is difficult.
- After 24 h, the hemostats may be removed and
the hemorrhage will have stopped.
- Vulvar or perineal lacerations can be sutured immediately
if seen at parturition, otherwise wait until all the swelling,
inflammation, etc. is gone.
- A laceration in the vaginal or vestibular areas may sometimes
become an abcess. They should be allowed to heal. Many times no
treatment is needed, especially if the dam is not systemically ill.
Caution should be exercised to not transport infective material into
uterus during anytreatments. (For example - a cow is found to have a
foul smelling vaginal discharge but the uterus is normal on rectal
palpation. A vaginal exam should be performed because if the source
is a vaginal tear or abcess, treating the uterus would drag the
infective material into the uterus.)
- Caruncles, if torn during obstetrical procedures can be the
cause of observed hemorrhage. Usually no treatment is needed.
- The umbilical cord will result in bleeding after it ruptures. This
is normal but if significant hemmorhage is observed, you should
verify that the ruptured cord is the source and there are no tears.
|
 Bovine
Index
Bovine
Index