Clinical
exam of the Mare
 79-95 79-95
- It may be obvious but identification of the mare should be
established, especially in cases where sale or purchase is involved.
Microchip or tattoo is preferred.
History
- A thorough history is essential in a reproductive exam of a mare.
It is important to consider the overall status of the mare.
- What is her age? Young mares, such as 2-3 yr olds are more likely
to have abnormal cycles. Old maiden mares may be more difficult to
get in foal.
- What has been her immediate past use? Hormone administration
associated with athletic performance (i.e. racing) may have a
detrimental effect on fertility, at least short term.
- What is her reproductive status? Is she a maiden, barren, or
foaling mare?
- Consider the stallion that is being used or will be used -natural
or AI breeding, fresh, fresh cooled or frozen semen? Is he fertile?
Obtain the year by year reproductive history.
- Have there been previous pregnancies and what was their outcome?
Consider anatomic changes associated with multiple foalings.
- Has the mare ever aborted? Is there any record of twinning? Has
she ever had dystocia? Has she ever has early embryonic death?
- Is there any record of postpartum complications such as retained
placenta or metritis? Has she ever had previous reproductive
surgery?
- What are the management conditions? What sort of teasing program
is used? How is breeding managed and what sort of treatments have
been used? Is lighting used to hasten cyclicity? Has she ever had
abnormal cyclic patterns?
Physical Exam
- The physical exam should begin with an assessment of the mare's
general condition, for example a long winter haircoat persisting
into spring may be associated with anestrus.
- Examine the external genitalia and perineum.
- Is there any
discharge?
- How is the vulvar conformation?
- The vulva should be
perpendicular to the ground with >70% of the vulva below the
ischium.
- The labia should form a good seal and close completely.
- The
"windsucker" test, performed by parting the vulvar labia
and listening for an inrush of air, tests the integrity of the
vaginal vestibular sphincter. Older, thin mares with a flat croup and atrophy of vulvar lips are
more prone to pneumovagina.
- The vaginal vestibular sphincter is
the most important of the barriers to contamination of the
reproductive tract. (The others are the labia and the cervix.)

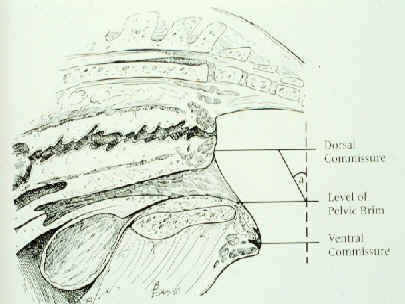
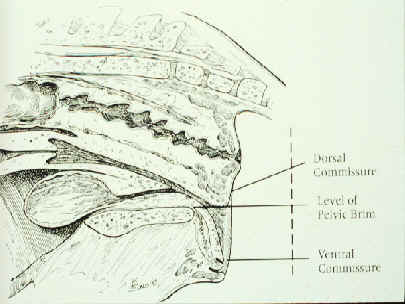
Examination of the conformation of the labia.
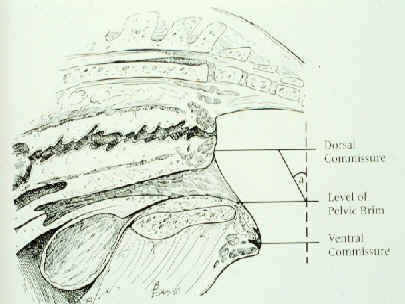
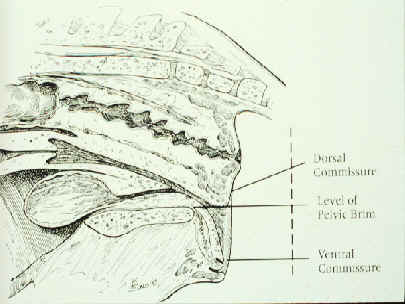
Locating the pelvic brim (left) and performing a
'windsucker test' (right).
Rectal Palpation
- The rectal exam is usually the next step. Proper restraint is
important.
- Students are usually concerned about rectal tears.
- The risk can be
reduced to some degree if proper restraint is used, adequate
lubrication is used and with proper manual technique.
- Just as
important is knowing what to do if one occurs.
- If a tear occurs or
is suspected, examine the tear (by speculum and manually)
immediately.
- Inform the owner what has happened.
- Determine if it is
a Grade 1,2,3 or 4.
- Treatment depends on the grade of tear,
economics, client, etc.
- Grade 1 tears (mucosa only) may not need
much treatment, maybe broad spectrum antibiotics and observation.
-
Grade 2 tears (muscularis only) may go unnoticed.
- Grade 3 tears
(everything but the serosa) are more serious and require treatment.
-
The aim is to prevent a grade 3 from becoming a grade 4.
- Initial
treatment should consist of broad spectrum antibiotics, tetanus,
anti-inflammatories, stool softening, anti-peristaltics (if
available) and packing the tear with medicated gauze.
- Many, if not
most of theses cases will go to surgery.
- Others may be treated
medically, just by replacing the packing periodically and
maintaining the antibiotics and stool softeners.
- Grade 4 tears (all
layers -full thickness) either go to surgery immediately or are
euthanized.
- The exam should be complete and systematic.
- The cervix reflects the presence of progesterone.
- If progesterone
is high, such as in pregnancy or dioestrus, it is long, firm and
tubular.
- When progesterone is low, such as in estrus or anestrus, it
becomes softer, flatter and shorter.
- In fact, when a mare is near
ovulation, it is very short, soft, and may be difficult to discern
- The uterus should be examined next.
- Always check for pregnancy
first!
- When examining the uterus, estimate the size of the uterine
horns and the tone.
- The tone of the uterus follows the cervix.
-
During estrus it is softer, with less tone, during diestrus it has
increased tone and a more tubular feel, during anestrus it is thin,
flaccid, and often difficult to palpate.
- The uterus should be
examined for contents (i.e. pregnancy, fluid) and consistency, such
as ventral enlargements at the junction of the horn and body,
atrophy, fluid, endometrial cysts (a common occurrence but often not
palpable), or a doughy, thick walled uterus (may indicate lymphatic
lacunae). Deep palpation of the endometrial folds may reveal areas
devoid of folds.
- After the uterus, palpate the ovaries.
- Evaluate the size (keeping
in mind seasonal effects), activity, structures present and their
size and softness.
- Follicles increase in size and become softer as
they near ovulation. I
- t is also helpful to record the location (e.g.
AP - anterior pole, PP - posterior pole, etc.) of follicles.
- Corpora
hemorrhagica (CH) can be palpated as well. Initially following
ovulation, a depression is felt.
- The mare may show pain on palpation
of a fresh ovulation.
- By 24 h after ovulation, the hemorrhage into
cavity forms a clot which may re-distend the structure.
- By 2 or 3 d
following ovulation, a CH and a follicle may feel similar, in which
case you may need to rely on behavioral signs and the cervix to
distinguish between the two.
- The mature (>5 d) CL cannot be
palpated due to retraction into the ovarian stroma.
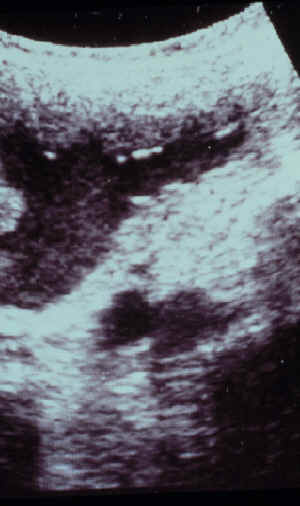
Ultrasound exam
- A key feature of the reproductive exam is the ultrasound exam.
With the ultrasound, you are able to see much more than you can
feel.
- Basically, the lower the MHz, the farther the image penetrates but
finer detail is lost; the higher the MHz, the image penetrates less
deeply but more detail is seen. With the ultrasound, not only can
ovarian structures be seen and easily measured, but their shape and
echogenicity can also be evaluated.
- Follicles not only increase in size as they near ovulation but
change shape, becoming more pear-shaped as they develop a tract
toward the ovulation fossa.
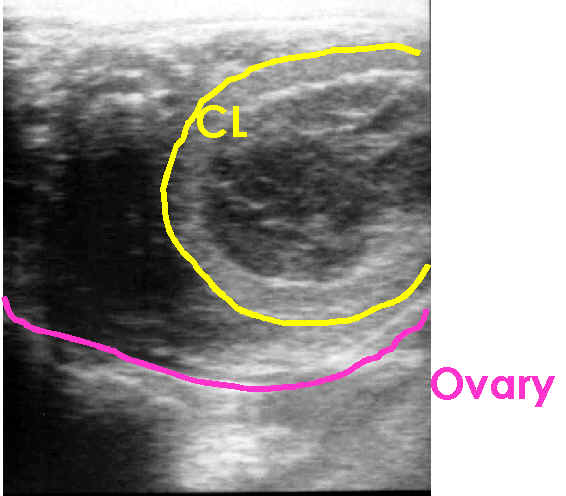
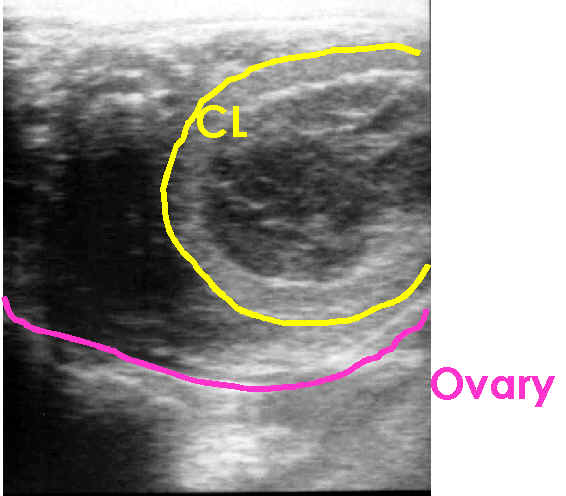
- An immature CL can easily be distinguished from a follicle.
- A CL can be identified with ultrasound even though it cannot be
palpated.
- Anovulatory follicles can be identified.
- Granulosa cell tumors can be differentiated from hematomas.
- Uterine size can be measured. Any contents can be identified. Even
small amounts of fluid can be identified as well the amount of fluid
measured and the character evaluated.
- Edema of the uterus is characteristic of estrus and is easily
recognized, endometrial cysts can not only be identified but their
size and location recorded for future reference.
- In short, an ultrasound examination is critical in the evaluation
of a mare and breeding management.
Equine Reproductive Ultrasonography: An
Overview
-
Ultrasonography has become an indispensable part of stud farm practice.
-
Ultrasonography is used for diagnosis and management in almost every
aspect of breeding management.
- In this overview of equine reproductive
ultrasonography, the organs examined, reasons for examination and some
possible findings will be briefly reviewed.
- More detailed information
will be provided in the lectures, discussions and laboratory sessions.
Ovaries
-
Examination of the ovaries can aid in determining the stage of the cycle
and in predicting or identifying impending ovulation.
Characteristics of the ovaries at the various stages of the estrous
cycle are:
- Anestrus: small ovaries, absence of a corpus luteum (CL), no
follicles > 20 mm
- Transition: ovaries of variable size, absence of a CL, follicles >
25 mm present
- Estrus: ovaries of variable size, absence of an active CL, may see
regressed CL, follicles > 25 mm present, usually 1,
occasionally 2, large (dominant) follicle present
- Luteal (Diestrus): early - evidence of recent ovulation; later -
ovaries of variable size, follicles may be present and can be large,
CL present
Ovulation
-
Various parameters have been investigated in an attempt to predict with
accuracy the time of ovulation. The importance of predicting ovulation
with accuracy increases with the use of shipped semen and becomes
critical when breeding with frozen semen. By palpation, the estimation
of follicular size and softness are the parameters used. With
experience, competency can be developed but there remains an element of
subjectivity and errors will occur with even the most experienced
palpators. For these reasons, objective criteria using ultrasonography
have been sought after. Unfortunately, at this time, no single reliable
criteria has been found which answers the need. Using a combination of
criteria will aid somewhat in the accuracy of prediction.
-
Increase in follicular size: Generally, follicles will increase in
diameter as they mature and approach ovulation. However, rate of growth
and maximum diameter reached will vary somewhat with season and between
mares. Maximum diameter will be slightly smaller near the summer
solstice. When measuring follicles, differences of 1 or 2 mm can be
found just by measuring slightly different points on the follicle on an
image, measuring different images of the same follicle or with 2
different operators. Therefore, general trends are probably more
beneficial than absolute measurements.
-
Change in follicular shape:
- Ginther reported that follicles will frequently develop a
"pear-shaped" appearance shortly before ovulation. The
"stem" of the pear is the tract the follicle develops leading
to the ovulation fossa. This characteristic shape is quite variable and
depends on obtaining the right angle with the ultrasound probe. That is,
if you slice a pear lengthwise through the base to the stem, it will
have a "pear-shape" but if you slice it at a right angle to
that, it will have a spherical shape. Likewise, the probe must be
positioned properly to get the "right slice". Moreover, not
all follicles can be seen to develop this shape leading up to ovulation.
-
Follicles initially appear nearly spherical. As they mature, the
follicle wall becomes thinner and hence the follicular shape is more
easily changed. For this reason, the shape of the follicle may appear
more elliptical or irregular as it matures and nears ovulation. The wall
of the follicles may appear less smooth as well. In other cases, the
follicle will maintain a spherical appearance until ovulation.
-
Echogenicity of antrum: Reports vary on the appearance of echogenic
particles before ovulation. In many cases, hyperechoic particles will
appear in the antrum close to ovulation. However, if these particles
increase in number and echogenicity, this indicates that the follicle is
likely to be anovulatory.
- It is important to be able to recognize ovulation. This is a key
event in the management of endometritis, scheduling pregnancy examinations,
etc. Because mares remain in estrus behaviorally after ovulation, many
mares are bred needlessly after they have ovulated. Detecting ovulation
will reduce unnecessary breedings, thereby reducing contamination of the
uterus and preserving stallion reserves for mares that need it.
-
Article - to
find out more
click here.
Corpus luteum
-
A very recent ovulation may be hard to detect upon examination.
- Within
12 - 24 hrs, it will fill in and have a hyperechoic appearance.
- The
equine CL has great variation in its ultrasonographic appearance.
- It can
have a homogenous echotexture or a trabecular appearance.
- The appearance
often changes somewhat as the CL matures. A CL may remain visible as a
smaller hyperechoic structure even after luteolysis.
-
Ovarian abnormalities
The section on ovarian abnormalities covers this area in more detail.
Uterus
-
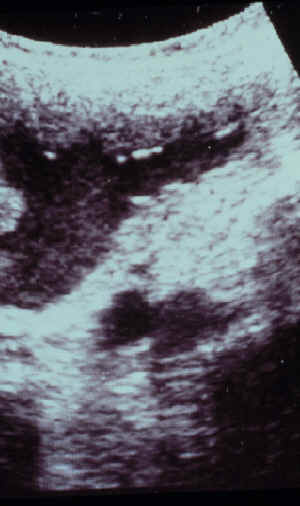
Examination of the uterus is extremely helpful in determining the stage
of the estrous cycle.
- Anestrus: the uterus is thin and elliptical, with a fairly
homogenous echotexture, bright spots indicating air are not uncommon
- Estrus: a characteristic pattern, giving the appearance of an
orange slice or wagon wheel, results due to the edema in the
endometrial folds
- Diestrus: edema is absent, the uterus is round (more so than
during anestrus), homogenous echotexture of the uterus
-
This is helpful when breeding a mare with shipped semen. For example, if
a mare is given prostaglandin and is presented for examination based on
the time lapse since the prostaglandin injection and the owner's
impression that the mare is coming into estrus, and upon examination has
a 43 mm follicle but no edema in the uterus - should semen be ordered?
Probably not. It may be that that follicle is going to regress and she
will build a new follicle, accompanied by uterine edema, in the next few
days.
Uterine pathology
-
The ability to view uterine pathology with ultrasonography is
indispensable in managing the infertile mare.
- Excessive uterine edema
and fluid in the lumen during estrus before breeding, retention of fluid
in the uterus after breeding, fluid in the uterus during diestrus are
all examples of pathologic problems that would go undiagnosed without
the benefit of ultrasound.
- As our understanding of endometritis has
developed the underlying importance of uterine clearance mechanisms is
felt to be central to the problem of post breeding endometritis.
- The
best way to diagnose this problem is with ultrasonography in the period
after mating.
- Fluid present in the uterus at 12 or 24 hours after
breeding is a clear indication for therapy to improve uterine clearance.
-
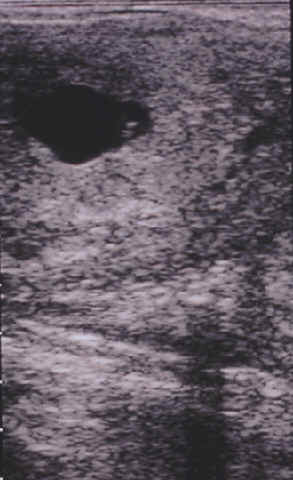
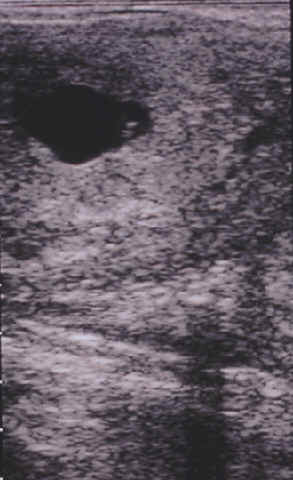
Endometrial cysts, although their role in infertility is somewhat
controversial, may cause problems in early pregnancy diagnosis and
identification of twins.
- During ultrasound examinations before breeding,
the location, size and shape of endometrial cysts should be recorded.
-
Photographic records are ideal.
- In this way, archival information is
available which will aid in future examinations and the ability to
discern a vesicle.
Pregnancy
-
Early detection of pregnancy is critical for good broodmare management.
-
The reasons for early detection are discussed more thoroughly in the
chapter on "Twinning in Mares".
- Basically, it not only
provides information on whether or not the mare is pregnant but allows
one to manage twin pregnancy in the most advantageous manner, may serve
to give early notice of a uterine infection and if not pregnant allows
mare time to arrange re-breeding.
- Normal development of the pregnancy can be monitored and it is
advisable for the practitioner to be familiar with the normal appearance of the
conceptus. For example, inexperienced users can sometimes mistake a
single conceptus with a developing allantois for twins. Knowledge of the
normal appearance and size of a conceptus may indicate an abnormality
which is likely to lead to early embryonic death.
- Fetal sexing can be
performed at approximately 60-70 d by the transrectal route and after approximately 100 d
by transabdominal approach.
Assisted Reproduction Techniques
-
Ultrasonography has opened up new possibilities for assisted
reproduction in horses.
- Oocyte collection for GIFT and IVF is based on
ultrasound guided transvaginal oocyte aspiration.
Vaginoscopic exam
- The next step is usually a vaginoscopic exam.
- The mare's cervix changes during the cycle.
- It is pink (estrogen
enhances the blood supply), edematous, relaxed (lying on the vaginal
floor near ovulation), and moist during estrus;
- pale, dry, and
closed (projecting out from the middle of the anterior vagina during
diestrus), often referred to as "high, white, and tight".
-
During pregnancy, it is pale, tightly closed and covered with a
sticky blue-gray mucus. During anestrus it is very pale, flaccid,
and may be open allowing you to see into the uterus.
Vaginal exam during estrus (left) and diestrus (right).
- Abnormal findings on vaginoscopic exam include pneumovagina, where
you may see the presence of debris or froth in the anterior vagina
and slight hyperemia; urine pooling which is usually most evident
during late estrus and is not uncommon at foal heat; vaginitis or
cervicitis; adhesions, scars, or lacerations; a persistent hymen;
exudates; and varicose veins.
Urine Pooling and a vaginal adhesion.
- The vaginoscopic exam may be followed by direct palpation of the
vagina, cervix and endometrium. You will be unable to completely
evaluate the cervix with a speculum and direct palpation of the
cervix is important to evaluate it for adhesions, lacerations, etc.
as well as the normal changes during the cycle. This is usually
performed at the same time as obtaining the culture and cytology
specimen. Direct palpation of the endometrium is not routinely
performed, especially since the advent of ultrasound.
Fiberoptic exam of the uterus, although not
a part of the routine examination, should be considered in problem mares
or when indicated by the history.
Folds of the uterus inflating (left and center) and the oviductal
papilla (right) where the oviduct enters the uterus.
Diagnostic procedures
Culture & cytology
- Culture & cytology of the uterus should be considered as a
single procedure.
- A culture without an accompanying cytology is worthless because it
is impossible to distinguish a contaminant from a pathogen.
- The best time to perform the procedure is during (late) estrus.
- It is absolutely essential that the swab used is a guarded swab.
An alternative to using a swab is a low volume flush.
Top to bottom: Kalayjian, Accu-CulShure, Tiegland.
Left to right : unguarded , guarded, guarded.
 Transport mechanisms. Transport mechanisms.
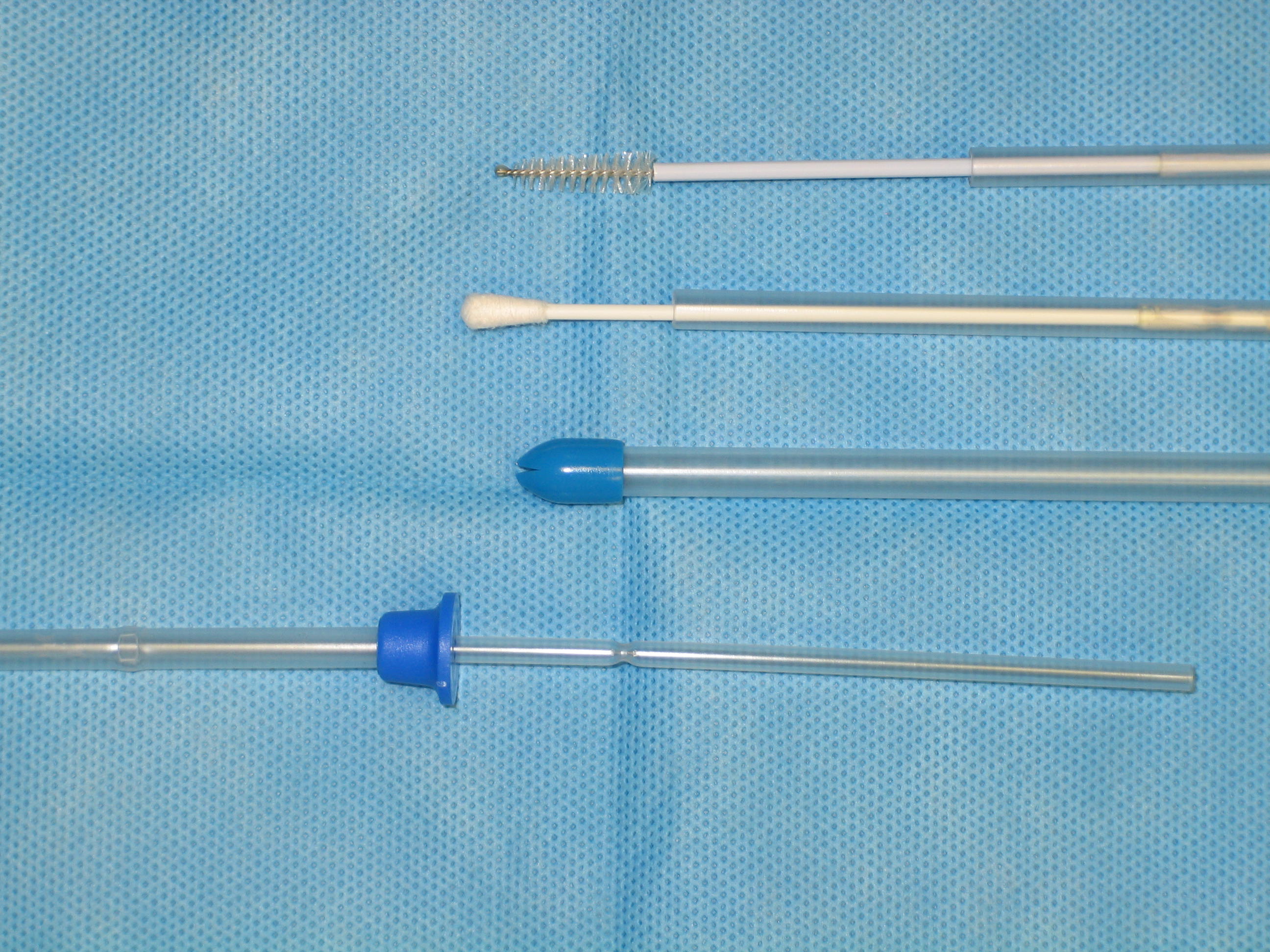
The culture/cytology system from Mini Tube that we use.
From top - Cytology brush with passer, Culture tip with
passer, Guarded Introducer, Introducer with passer (end you hold)
- While studies have shown no difference for normal mares, in
subfertile mares there were fewer positive cultures and fewer
positive cytologies with a swab than with a flush.
- Culture results must be correlated with cytology findings and
pathogens differentiated from non-pathogens.
- A positive culture with a negative cytology should be disregarded
as a contaminant. A positive culture with a positive cytology should
be interpreted as isolation of a pathogen and sensitivity performed.
- A negative culture and positive cytology may indicate
noninfectious inflammation or a problem with sample handling.
Low
volume
flush
cultures
- Recent work (as well as some older work) has shown this may be more sensitive at diagnosing mares with uterine infections.
- Insert a Bivona catheter through the cervix (do not inflate the cuff)
- Flush 60 mL of saline into the uterus using a catheter tip syringe and retrieve after 30 second uterine message per rectum into drained into a sterile 50 mL conical tube3 by gravity flow.
- An aliquot (4 mL) of the sample was placed in a 5 mL sterile tube for measuring pH.
- centrifuge remaining sample at 500 rpm for 10 min. and decant all but 5 mL of the supernatant
- Insert a sterile culture swab into the pellet for subsequent microbiologic culture.
- Use a second sterile swab rolled onto a glass slide for cytological examination.
Biopsy Cultures
- Some prefer to culture the biopsy
- Strep can be present deep in tissue and not on surface
Endometrial biopsy


Obtaining a biopsy. Pass the biopsy instrument manually through the
cervix, pull your hand out and place your hand in the rectum, push a
fold of endometrium into the jaws, close the jaws and tear out the
biopsy sample.
- The endometrial biopsy is usually the last step in the
breeding soundness examination. It is indicated in prepurchase
exams, barren mares and mares requiring reproductive surgery, among
others.
- When to perform a biopsy is a matter of choice and availability.
-
During estrus the cervix is open and more easily penetrated and the
mare is more resistant to endometritis, while during diestrus the
endometrial glands are more active and may give a better picture of
their function.
- Early work indicated that one site was representative, however we
now know that there may be significant differences between sites in
a uterus. Therefore, in deciding where to obtain the biopsy, if
palpation or ultrasound indicates an abnormal area, biopsy that area
as well as a normal area. Otherwise, choose a site at random, being
sure to stay away from the cervix and area near the internal os.
- To be able to interpret the biopsy, it is important to obtain an
adequate sample.
- Modified Davidson's solution may be better the formalin or Bouin's to fix the sample.
- (30% of a 37-40% solution of formaldehyde, 15% ethanol, 5% glacial acetic acid, and 50% distilled H2O)
 Adequate biopsy size. Adequate biopsy size.
Inflammation
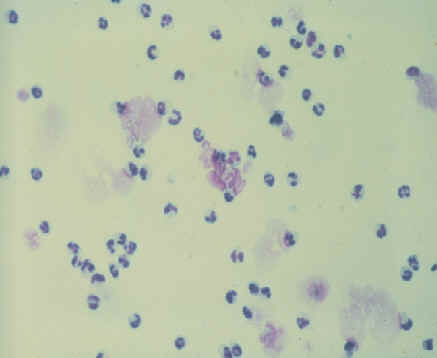
- The biopsy is examined for signs of inflammation.
- Neutrophils will
be present in the acute stage while lymphocytes and macrophages are
seen in chronic inflammation.
- Eosinophils are associated with fungal
infections or pneumovagina.
- In addition, the biopsy is evaluated for
the degree of fibrosis (absent, mild, moderate, severe) based on the
number of layers and the frequency of lesions (how widespread).
Fibrosis and nesting
- Glandular nests are recorded, and whether fibrotic or physiologic.
-
Physiologic nests occur during anestrus and transition and can be
differentiated by the absence of layers of fibrosis around the
glands.
- Periglandular fibrosis around individual glands is evaluated
as well (scattered, widespread, frequent, occasional, number of
layers).
 Fibrosis around glands. Fibrosis around glands.
Other evaluations
- The endometrial epithelium is evaluated and the tortuosity of
glands (more tortuous under the influence of progesterone). Any
indications of endometrial atrophy are noted. Endometrial atrophy is
considered abnormal during breeding season and may be localized in
older mares. Cystic (dilated) glands are noted. These are
nonfibrosed glands distended with inspissated secretions and are
common during anestrus and transition.
- Siderocytes are an indication of previous pregnancies.
- Lymphatic lacunae are evidence of abnormalities in lymphatic
drainage and are important factors in infertility. The pattern of
lesions is noted. Widespread lesions are numerous and appear widely
throughout the sections. Scattered lesions are few and irregularly
distributed. Discrete foci are concentrated changes with rather
sharp, well-defined margins. Diffuse foci are spread out with
indefinite margins.
Grading
- The biopsy is assigned to a category based on the evaluation.
- The categories are: I - essentially normal, pathologic changes
slight and sparsely scattered; IIA - mild changes; IIB - moderate
changes; III - severe changes.
- The effects are additive and if a mare is barren > 2 yr
the score is increased one grade. More information on criteria for
evaluating a biopsy and placing it into a category can be found in
the chapter by Kenny and Doig in Current Therapy in Theriogenology
II. The categories have been associated with the expected foaling
rate.
- Category I mares have an expected foaling rate of 80-90% and the
foaling rate reflects the overall management.
A grade I biopsy.
- Category IIA mares have an expected foaling rate of 50-80% and the
foaling rate reflects overall management plus endometrial changes.
- Category IIB mares have an expected foaling rate of 10-50% and
again the foaling rate reflects overall management plus endometrial
changes.
- Category III mares have an expected foaling rate of 10% and the
foaling rate reflects severe changes in the endometrium.
|


 Transport mechanisms.
Transport mechanisms.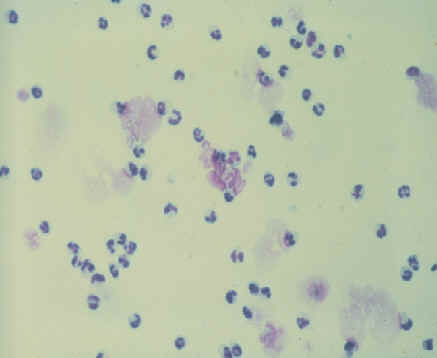
 Adequate biopsy size.
Adequate biopsy size. Fibrosis around glands.
Fibrosis around glands.



 Equine
Index
Equine
Index