|
Equine
Pregnancy
 103-153,
157-165, 177-178 103-153,
157-165, 177-178

Physiology of
Pregnancy
The Early
Embryo
-
At about 24 hours post
ovulation the embyro is at 2 cell stage
-
4-5 days - morula
-
5-6 days blastocyst
-
5-6 days enters uterus
and zona shed
-
Capsule forms at
blastocyst stage

-
Migration to day 16. The
embryo migrates in the uterus for approximately 16 days to release a
'signal' that pregnancy is established. Fixation
of the embryo (gestational sac) occurs at about 16 days post ovulation.
Endometrial cups
-
At
about 36-38 days, fetal tissue along the chorionic girdle begin to invade
the endometrium and form the endometrial cups.
-
Endometrial
cups secrete eCG ...Equine Chorionic Gonadotrophin (formerly PMSG...Pregnant
Mare Serum Gonadotrophin). This acts to
luteinize the normal follicular waves that are occurring and results in
formation of the secondary corpora lutea.
-
The
cups remain, even if the pregnancy is
lost, and are then sloughed at the
normal time (120 days).
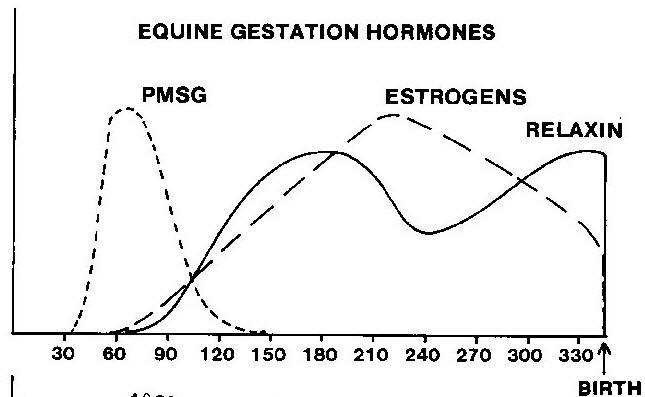
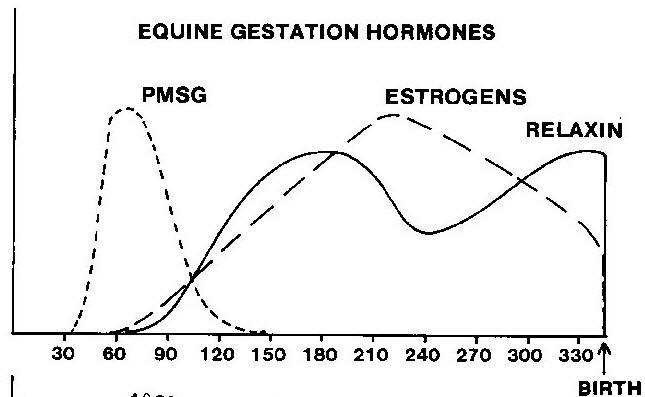
Equine chorionic gonadotropin (eCG): (formerly
pregnant mare serum gonadotropin or PMSG)
-
Produced by the endometrial cups beginning around d
37-42, peaking around d 60-80, after which the endometrial cups start to
decline, disappearing around d 120-150.
-
The function of the endometrial
cups and eCG are unclear.
-
Some hypothesize an immunologic role in helping to
maintain pregnancy.
-
Causes luteinization of follicular waves to create
secondary CLs.
-
Although eCG has an FSH-like action in many other
species, it has LH-like activity in mares.

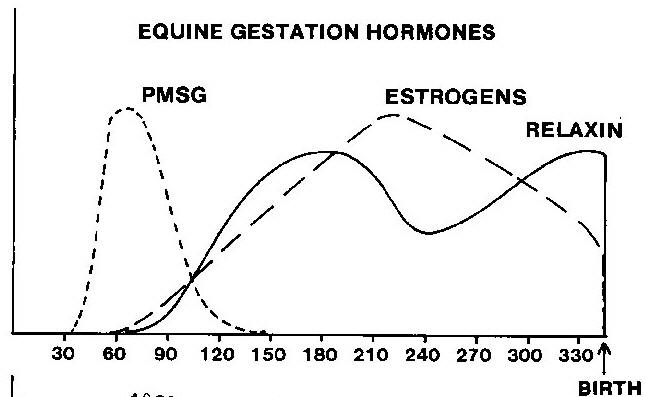
Secondary CLs
- The
secondary CLs result in progesterone rise about day 60-120. The
endometrial cups regress (they are sloughed from the uterus by an
immunologic response).
- Secondary vs. accessory CLs (ovulatory
or anovulatory)
Progesterone/Progestagens:
-
Progesterone initially rises, followed by a slight decrease then rises to a peak at d 80, then gradually declining to 1-2 ng/ml during mid-late
gestation (d 150).
-
The second rise is associated with the formation of
accessory and secondary CL.
-
The 5 alpha pregnanes rise from mid
gestation to term.
- Produced from maternal cholesterol
-
The fetoplacental unit produces sufficient
progestagens so that ovariectomy can be performed after 120-150 d.
- Late gestation progestagen rises (last month of
pregnancy)
- From fetal adrenal production of 5
alpha reduced pregnanes (adrenals do not have 17 alpha
hydroxylase)
Estrogens
- Mare
ovarian estrogens begin to rise at day 38-40.
- From gonadotrophic stimulation of luteal
tissue
- Late in
gestation maternal estrogen production rises.
- At
day 70-80 a second rise of estrogens from the fetal-placental unit occurs.
-
Placental aromatization of the common C-19 precursors
-
dehydroandrosterone (DHA) and dehydroepiandrosterone (DHEA)
-
Secreted by fetal gonads.
Placenta
- The
placenta takes over progestagen (not progesterone) production until
foaling. Therefore, a mare does not need her ovaries after about 120
days of gestation.
- The mare has diffuse type of microcotyledonary
placenta
- Complete placental formation is done at 150
days.
|
Equine Placentation adopted
from Ginther |
  |
Day 9-10
Inner cell mass (brown)
Yolk sac starting |
 |
Day 14
Still mobile
Mesoderm will be blood vessels and connective tissue.
|
 |
Day 16
Folds start to form over embryonic disc to form amnion. |
  |
Day 48-19
Amnion has formed.
Note the two and three layered areas.
|
 |
Day 21
Allantois is emerging. |
 |
Day 25
Allantois has moved over embyro.
Heart beat present.
Note red developing chorionic girdle. |
 |
Day 30
Note red chorionic girdle which will form the endometrial cups. |
 |
Day 40
Embryo moved to opposite pole.
Yolk sac replaced by allantois. |
 |
Day 80
The yolk sac is only a remnant.
Conceptus fills both horns. |
Pregnancy
Diagnosis
- Certain characteristics
of pregnancy in the mare aid in diagnosis.
- Progesterone causes increased
tone of the uterus and cervix.
- Estrogen from the conceptus, in
conjunction with the progesterone results in exaggerated tone.
- The
vesicle is spherical and distinct, and can be palpated from 18 d (+)
through 60-70 d, and seen with ultrasound beginning at 10 or 12 d
(depending on the machine).

-
Other significant characteristics of equine pregnancy
include the presence of chorionic girdle cells from the fetal
trophoblast which invade the endometrium. The ovaries are active during
pregnancy, with large follicles palpable especially around 18-23 d and
36-45 d.
Hormones
Estrogens
Click on the BET labs icon to see their web page and find out what
hormones they run.
External signs of pregnancy
- Although
abdominal enlargement is characteristic of pregnancy, it is unreliable
as a diagnostic sign.
- Ballotment or observed movements of the fetus can
often be seen late in gestation.
- Mammary changes are quite variable.
-
Pelvic changes (relaxation of the pelvic ligaments) occur late in
gestation but are often difficult to detect.
-
Cessation of estrus
behavior is variable and unreliable.
- Some mares will continue to show
estrus even when pregnant.
Methods of
diagnosisPalpation
per rectum
- Cervical changes from 16 or 17
d to term are elongation, firmness and tubularity. The uterus also has
increased tone.
- The chorionic vesicle is distinct and spherical
and approximate sizes are:
- 28 d (4 wks)
Key lime (pullet egg)
- 35 d (5 wks) lemon
-
42 d (6 wks) orange
- 49 d (7
wks) grapefruit
- 56 d (8 wks) cantaloupe
-
By 90 d it is hard to delineate the cranial margin of
uterus.
- Fetal Ballotment per rectum becomes
consistent after 150d.
- Aging fetus by size, as
in the cow, is imprecise.
- Differentials which
may confuse the examiner include the bladder and enlargement in the non
pregnant tract at the base of the uterine horn.
Ultrasound
- The
time of earliest diagnosis depends on the MHZ of the probe.
- Gestational
age can be estimated from the size of the vesicle.
- There is a plateau in
the growth curve between d 17-24 during which the size does not increase
much.

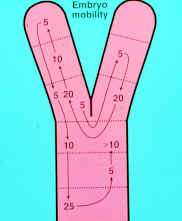
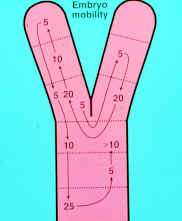
- Movement of the
vesicle is characteristic of early pregnancy, covering the entire uterus
and moving surprisingly rapidly.
- Movement ceases around d 16-17 when
"fixation" occurs.
Movement of the equine embryo.
-
The fetal heartbeat can be observed around d 23-24.

- The vesicle
undergoes a series of changes, having a very characteristic appearance
at various stages with which the examiner should be familiar.
- The
vesicle usually becomes fixed in a location at the base of a uterine
horn.
- Although initially spherical, the shape becomes more triangular
around d 18 and the embryo becomes visible around d 20-21, usually in a
ventral location.
- Changes in the shape of the vesicle and the
characteristic location of the embryo are related to the developing
trophoblast.
- At d 21, the embryo is at the bottom of vesicle and the
entire hypoechoic structure is the yolk sac.
- Soon thereafter the
developing allantoic membrane can be seen.
- By d 30 the embryo is found
in the middle of the vesicle suspended by the developing allantoic
membrane, with the allantoic sac beneath and the yolk sac above.
- By d 36
the embryo is near the top of the vesicle and the yolk sac is all but
gone.
- By d 40 the embryo is back in the middle of the vesicle, suspended
by the umbilicus.
-
Vesicles that are smaller than
normal size for their age are associated with increased rates of
embryonic loss.
-
One of the critical reasons for a thorough early
pregnancy exam is to detect twins, which will be discussed in more
detail later.
Fetal sexing
-
Fetal sexing is becoming more and more in demand.
-
Numerous reasons exist
for owners desiring knowledge of the sex of the fetus, such as
appraisals, insurance coverage, payment of stud fees, sales
consignments, mating lists, sale or purchase, etc.
-
The veterinarian
performing fetal sexing should be aware of the liability implications
involved.
-
Gender determination is based on the location of the genital
tubercle.
-
The genital tubercle is the precursor of the penis in the male
or the clitoris in the female.
-
The tubercle migrates toward the
umbilicus in the male and toward the anus in the female.
-
Ideal times for
performing the procedure are from 59 to 68 days or 5 to 6 months.
-
Before
58 days the tubercle is not distinct enough and has not migrated
sufficiently to make a distinction.
-
After 70 days the fetus is hard to
reach until it is approximately 3.5 to 4 months of age.
-
As the fetus
gets larger, a trans-abdominal approach may be preferred.
-
It is important
to mention that accuracy is based on certainty and that the veterinarian
should keep their own written records. If cattle are available, it is
easier to learn the technique on cattle because the manipulations are
easier and they are more tolerant of prolonged rectal examinations.
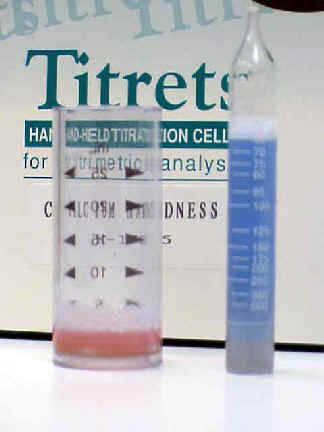
Indirect pregnancy tests
-
The
presence of eCG has been used as a test for pregnancy because it is only
found in pregnant mares.
-
The problem is that it remains elevated after
the cups are formed even if fetal death occurs. In house tests are
available which makes them attractive in some situations (e.g. miniature
horses).
-
For example, with the Synbiotics test, it is reported that 20%
of samples are positive at 30 d, 66% at 38 d, 76% at 40 d, and 92% at 42
d.
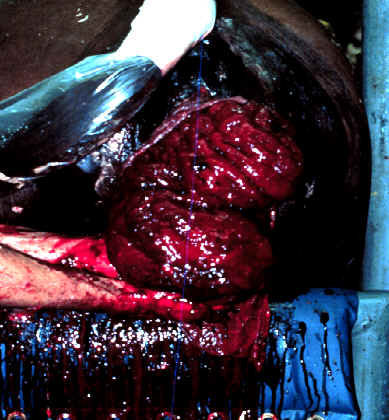
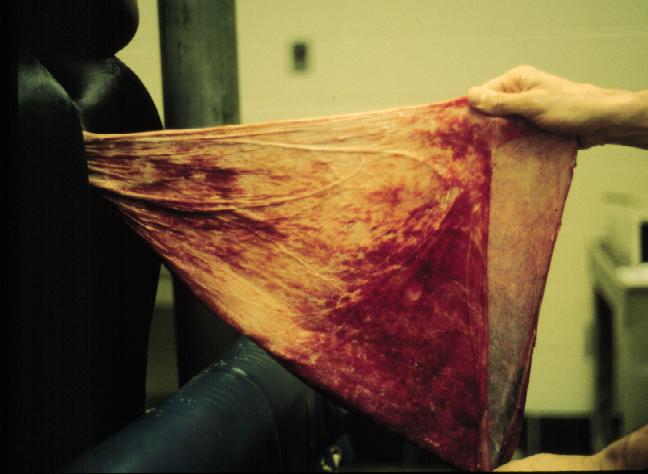
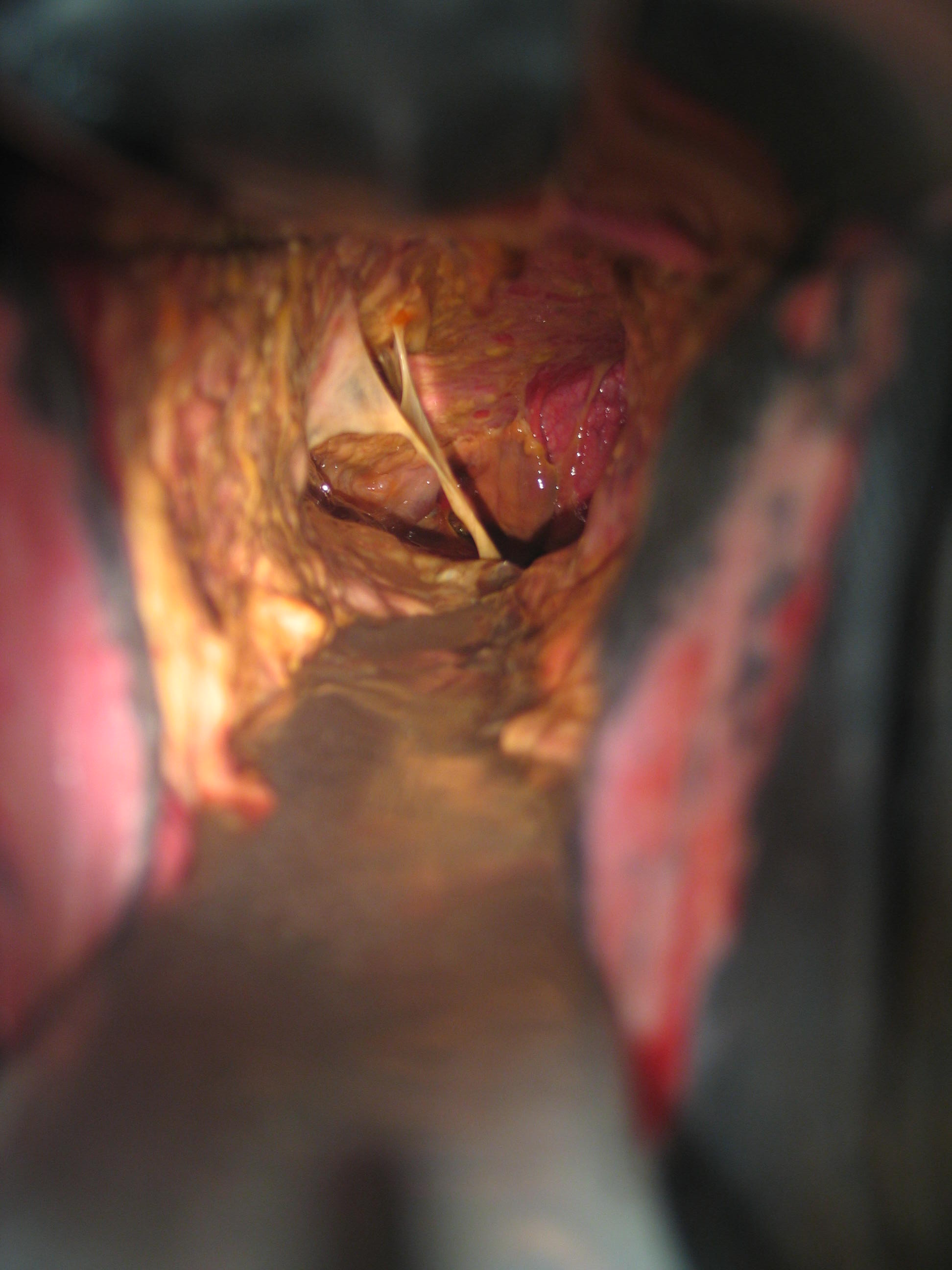
Endometrial cups in a mare.
-
Estrogens are elevated 150 d to term
(due to
production from
fetal gonads).
-
The Cuboni
test, based on fluorescence of urine, is 90% accurate after 100 d,
100% accurate after 150 d.
-
Generally, that late in gestation, other
means of pregnancy diagnosis have already been employed.
Cuboni test.
-
Estrone sulfate can be tested for in almost any
bodily fluid. In serum there is a sharp rise after 60 d, peak levels by 80
d.
-
Before 60 d a false positive can be obtained due to estrus. In milk a
similar pattern is observed, only with lower values.
-
It is
considered
an indicator
of fetal
viability
after 44 d.
In feces, it
can be found
after 4 mos.
And can also
be found in
urine.
Testing is noninvasive and therefore
used in studies of wild equids.
-
Commercial tests available "Equi Test - ES" (www.trideltaltd.com);
"Confirm"
(http://www.icpbio.com/site.aspx/Pages/Products/ConfirmEquine)
-
Early
Pregnancy Factor
Check
this link out to a potentially exciting method to determine
pregnancy.
- EPF - two components
- EPF-A - Uterine tube
- EPF -B - Ovary
- Production requires signal from fertilized ovum (ovum factor)
released under prolactin presence after sperm penetration.
- Appears 4-6 hours
- Disappears with fetal death
- Non-detectable at 20 days in milk and 30 days in serum
- Lateral flow dipstick test
- It does not work in the cow, so I have
doubts in the mare.
- I have seen no refereed papers about its use
in the mare.
Problems of
Pregnancy
Uterine
torsion
- Uterine torsion is an uncommon
problem, found usually late in gestation (7 mo to term) but not usually
at parturition (unlike the cow).
- It is thought that the reduced
incidence in the mare can be attributed at least in part to anatomical
differences from the cow in the attachments of the uterus to the body
wall by the broad ligament and to the method of rising (front end first
as opposed to cow).
- The clinical signs are those of colic.
- Diagnosis is
made by rectal palpation.
- The broad ligaments are crossed, one going
over the uterus, the other below.
- The location of the ovaries is
abnormal as well.
- A vaginal exam is usually not very helpful, as the
vagina and cervix are rarely involved.
- Treatment is generally surgical
via either a standing flank laparotomy or midline laparotomy.
- After
correction, the pregnancy is allowed to continue to term.
- Rolling has
also been reported (JAVMA 193:3, p337).
- In that report, 6 of 7 were
successfully corrected, with 1 uterine rupture (355 d gestation,
previous attempt at correction).
Prepubic tendon rupture
- More
commonly seen in older, heavier (draft) mares, it is not common in
athletic breeds.
-
There is
probably not
really an actual
pre-pubic
tendon. It is
really a tear in
the muscle.
- The first sign is ventral edema.
- This is followed by a
"Dropped" abdomen.


- The mammary secretions may become bloody.

-
Treatment consists of abdominal support and reducing activity.
Parturition or induced or assisted or an elective C-section
has been the
traditional
treatment. A report from U Penn
(JAVMA
232:257-261,
2008) indicates that a
conservative
approach (wait
and let the mare
foal) may result
in better mare
and foal
prognosis.
- The prognosis is poor for survival of
both the dam and the fetus.
Obstetrics
- Normally parturition occurs at night,
and the mare seemingly can delay parturition until the setting suits
her.
- Horses have a very variable gestation length (ave 335, range
305-405).
- It is a very rapid process. Often being completed in less than
20 min.
Signs of impending parturition in the
mare
- Udder development is evident 3 to 6
wks prior to foaling.
- "Waxing" or the presence of a very thick
drop of sticky colostrum at the teat end, can be observed 1-72 h prior
to parturition.

- Some mares may leak colostrum for days, to the extent
that insufficient good quality colostrum is available when the foal is
born.
- There is slight relaxation of the sacrosciatic ligaments but this
is not as evident as in cows, especially in the heavily muscled breeds
like Quarter Horses.
- The vulva becomes edematous and lengthens.
- Most
importantly, there is a change in the electrolytes in the mammary
secretions.
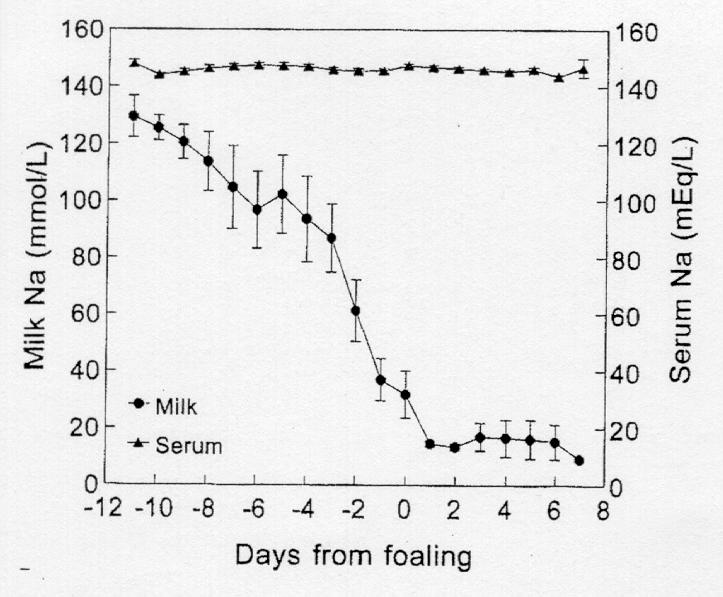
- Potassium and magnesium increase,
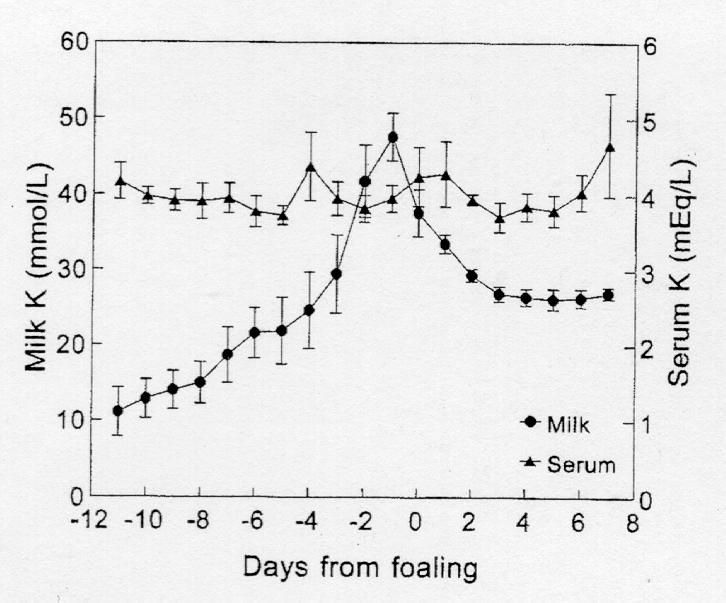
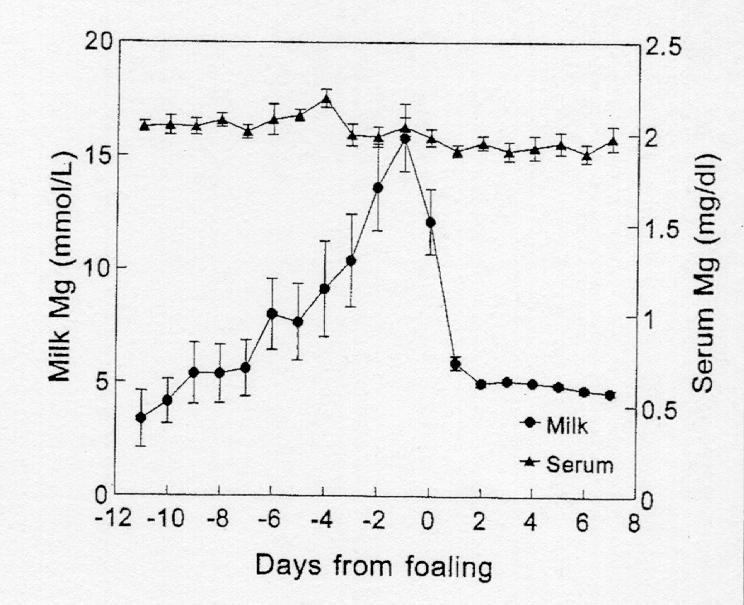
- Calcium increases sharply.
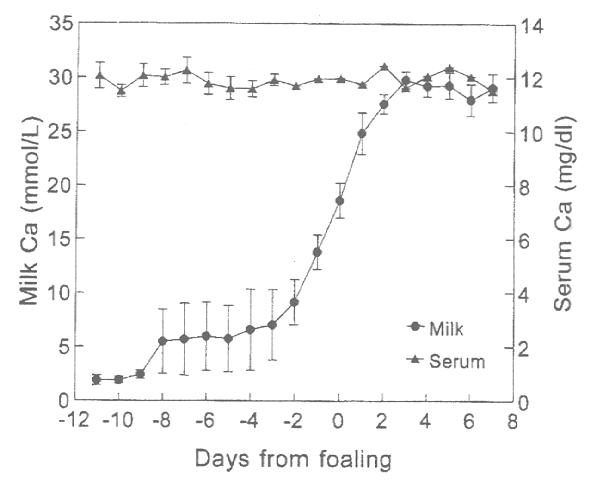
- A point system based on these changes was
developed by Ousey et al. to aid in predicting foaling. Others watch for
the crossing of the sodium and potassium curves in addition to elevated
calcium.
|
Calcium
mmol/L
|
Sodium
mmol/L
|
Potassium
mmol/L
|
Points |
|
> 10 |
< 30 |
> 35 |
15 |
|
> 7 |
< 50 |
> 30 |
10 |
|
> 5 |
< 80 |
> 20 |
5 |
- The most important
change is an increase in divalent cations (Ca++, Mg++) in milk.
- The
increase in magnesium is more gradual and occurs earlier pre-partum
than Ca++. It is the increase in Ca++
that is most useful.
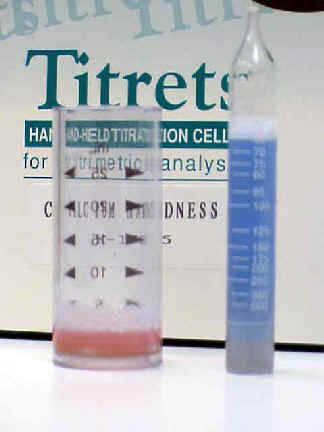
- When calcium rises >10 mmol or 400 ppm,
parturition is imminent.

Characteristics of parturition in mares
-
Stage 1 is characterized by restlessness, walking,
frequent urination, sweating, the mare is anxious, looking at her
abdomen, getting up and laying down, rolling.
-
Most mares will rise at
least once after going down, but repeatedly getting up and down may
signal a problem.
-
The foal has an active role in its final positioning,
going from dorso-pubic to dorso-sacral.
-
The duration of Stage 1 is
usually about an hour or a little longer (10 min - 5.5 h).
-
Stage 1 ends
with the rupture of the chorio-allantois at the cervical star.
- Stage
2 consists of 15 to 30 min of very forceful expulsive efforts.
- The foal
is presented in the intact amnion, usually with one forelimb about 6 in.
behind the other.
- The long umbilical cord remains intact until the mare
rises.
- It was once thought that significant blood flow, up to 1 liter,
occurred through the cord after birth and people were cautioned about
breaking the cord too soon.
- However, more recent studies have shown that
there is no significant blood flow in the cord after birth and there is
no difference in the PCV between foals in which the cord is broken soon
after birth and those in which the cord is left intact.
- Stage
3 typically appears as a tranquilizing effect post-delivery.
- The
placenta is usually passed in less than 3 h after parturition.
- After
delivery, the navel should be disinfected with 2% chlorhexidine.
-
Non-tamed iodine is associated with an increased incidence of patent
urachus, and other problems because it is too harsh.
- Povidone iodine
does not disinfect adequately.
- Good colostrum
has a specific gravity >1.06 and adequate intake should be observed.
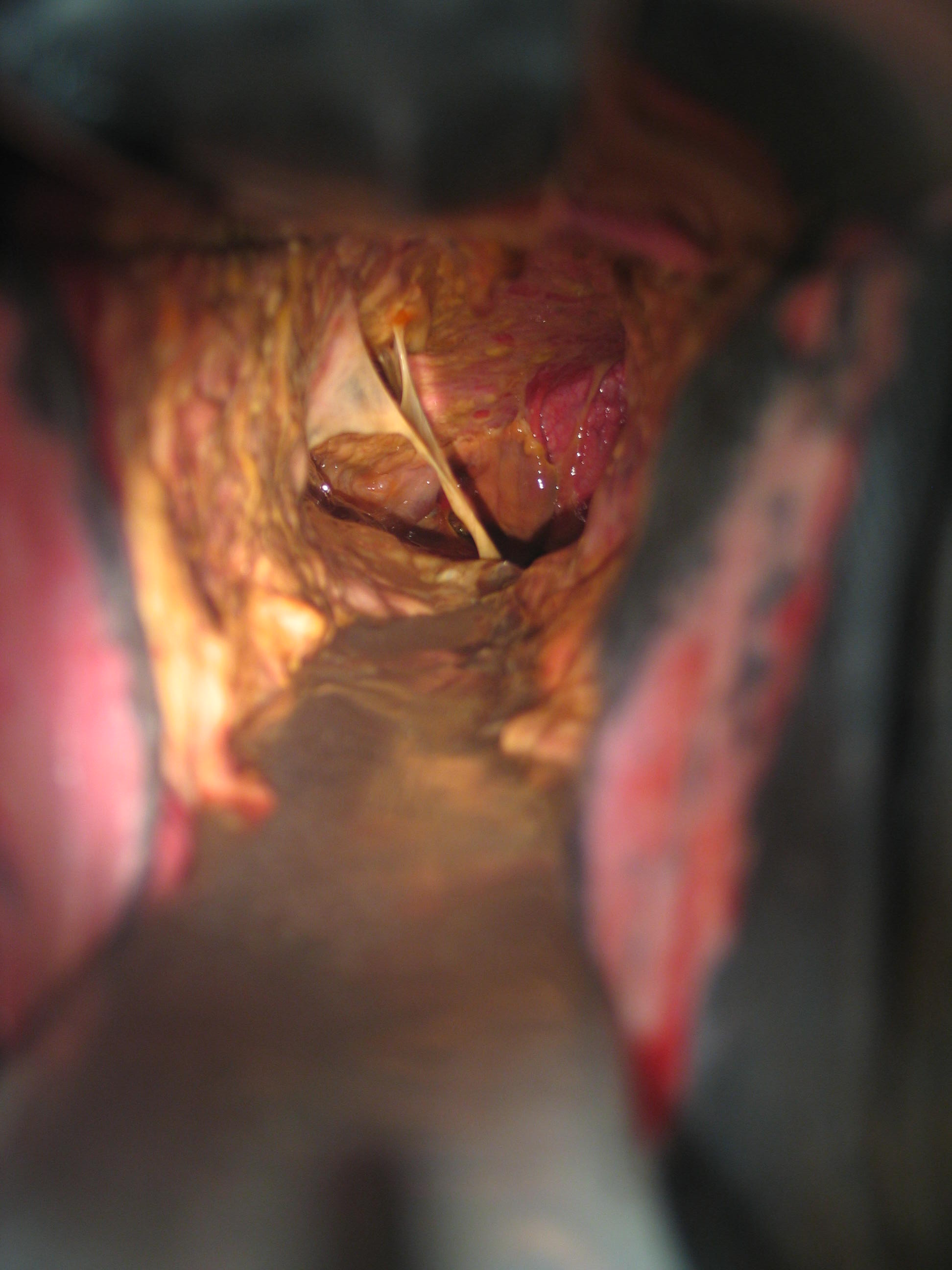
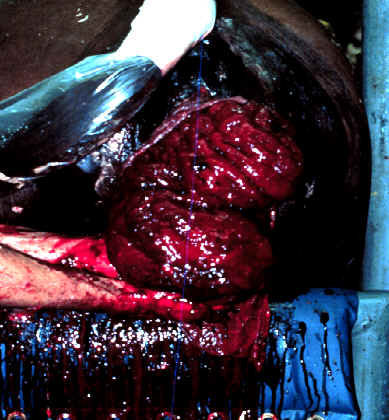
Inspection of the placenta should be routine.
-
Make
sure that all the placenta has been passed.
-
Check for signs of
placentitis. Any abnormal areas may indicate septicemia of the foal.
-
Treatment should begin immediately, before clinical signs appear in the
foal. Also check for other abnormalities in the placenta. Areas of
aplastic or hypoplastic villi are an indication of uterine pathology.
Dystocia
- Considerations
to keep in mind in the management of dystocia are that the process of
parturition is very rapid and very forceful.
- The reproductive tract of
the mare is easily traumatized. Mares can be unpredictable during
dystocia and it is advisable to use caution.

Guidelines on when to intervene:
-
After 10 min of strenuous labor and no sign of the
fetus perform an examination.
-
If the forefeet and muzzle are in the
canal, allow the mare to continue.
-
After strenuous contractions for
another 10 min, assist delivery.
-
The amnion, which is a white membrane,
should protrude from the vulva within 5 min of rupture of the
chorio-allantois.
-
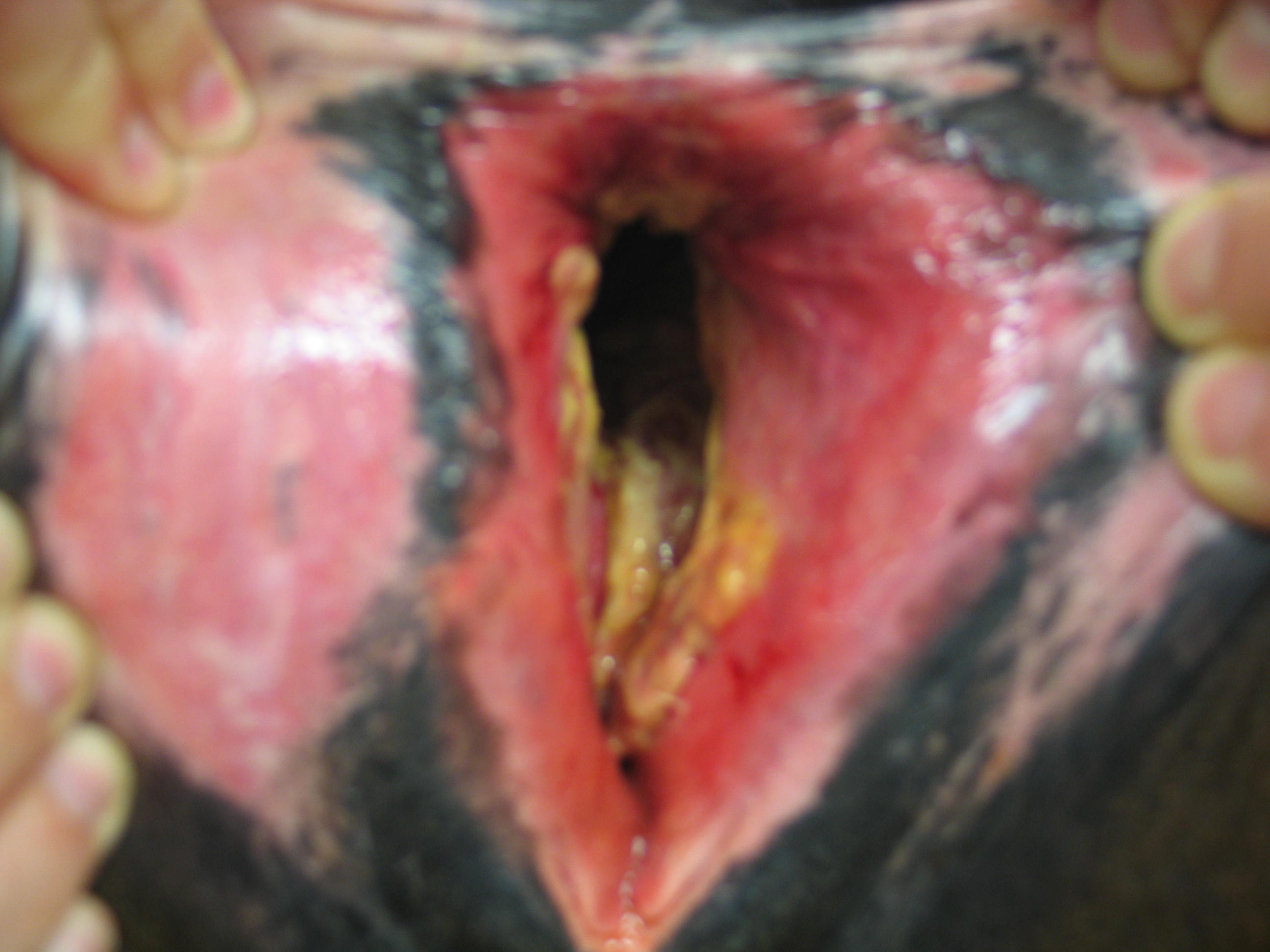
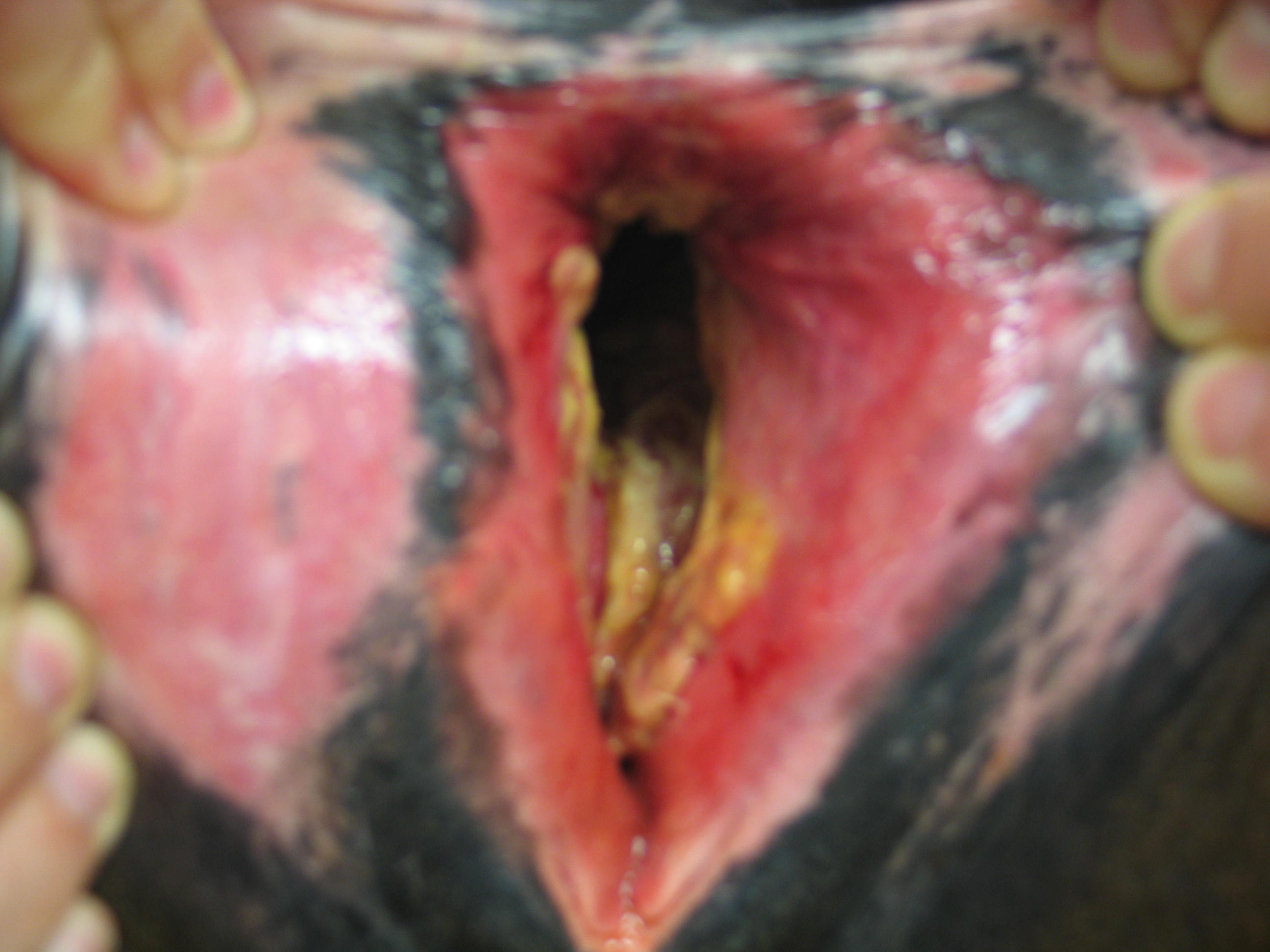
If a red velvety membrane (the chorio-allantois) is
seen at the vulva, a true emergency exists. This is termed 'red
bag'.
-
Unfortunately, if
intervention is needed, oftentimes the foal will be dead.
-
Assistance
must be given rapidly if the foal is to be saved.
-
A weak or dead foal
cannot assist in the process of parturition.
Proper restraint, both physical and chemical are
important.
- Minimize the use of drugs that
will affect the CNS and cause respiratory depression of the foal.
- For
sedation or tranquilization, acepromazine is not recommended if the foal
is alive because of its long clearance time.
- Barbiturates are also not
recommended because of severe fetal depression, even with doses that
don't affect the mare.
- Both xylazine and detomidine can be reversed with
yohimbine (0.05 mg/lb, IV).
- Caution should be exercised if xylazine is
used alone as it will sometimes result in hypersensitivity of the
hindquarters.
- Epidural anesthesia is not recommended because it takes
too long to take effect, doesn't stop the abdominal press and may cause
the mare to be unstable in the hindquarters if she ends up needing to be
shipped somewhere or during recovery if she undergoes general
anesthesia.
- Short term field anesthesia can be
accomplished with xylazine (1 mg/kg IV) or detomidine (10 µg/lb, IV)
followed by ketamine (2 mg/kg IV) after the mare drops her head. Then
administer "triple drip": 5% glycerol guaiacolate (GG)
solution containing 0.5 mg/ml xylazine (or 20 µg/ml detomidine) plus 1
mg/ml ketamine administered at approximately 1.0 ml/lb/hr (if give a
second bag use 0.25 mg/ml of xylazine).
- If the
foal is dead, you can use glycerol guaiacolate and thiobarbiturate.
-
For Caesarian section: give GG (5% Sol.) to effect,
then ketamine (1mg/lb) then intubate (Isoflurane preferred over
Halothane); if pre-medication is desired, 50 mg valium can be given IM,
10 mg butorphanol IV.
- After delivery, give the
foal Dopram (0.2 mg/kg, IV) and yohimbine if needed.
Cleanliness and lubrication are absolutely
essential in the management of equine dystocia.
- Petroleum
jelly is a good choice of lubricant.
- Water soluble lubricants are
acceptable but must be replenished more often.
- Do not use a detergent as
a lubricant because it has a de-fatting action on the tissues.
-
Do
not
use
J-lube,
particularly
if a
C-section
may
be
anticipated.
J-lube
has
been
found
to
be
quite
toxic
if
in
the
peritoneum.
Prompt assessment of the cause of dystocia is
important as is relatively rapid decision making as to the course of
action.
- Abnormal fetal posture is the most
common cause of dystocia because of the long extremities and neck of the
foal.
- Normally, the foal is an active participant in parturition.
- A weak
or dead foal fails to participate in the process.
- Congenital deformities
such as wry neck, contracted tendons or ankylosis result in dystocia.
-
Dog sitting posture, foot-nape presentation (often causing a
recto-vaginal laceration if not corrected) and nape presentation are
fairly common problems.
- Abnormal presentation, e.g. posterior or
ventral-transverse also may be encountered.
- Twins frequently result in
dystocia.
- Maternal causes, such as a tight vaginal-vestibular sphincter,
a small vulva or Caslick's that was not opened may also be involved.
Premature separation of the chorio-allantois (or
"red bag" in lay terms) is an obstetrical emergency.
- This
can be recognized by the appearance of a red, velvety membrane at the
vulva before delivery of the foal.

- The chorio-allantois must be ruptured
immediately and delivery assisted because the foal will rapidly become
hypoxic and anoxic.
- Clients should be made aware of this condition
because if they do not take action and await the arrival of a
veterinarian, the foal will die of anoxia.
- Premature placental
separation is associated with placentitis (the placenta is too thick to
rupture at the cervical star area), twinning, inappropriate induction
methods (PGF) and unknown causes.
- In many cases, the mare doesn't strain
and the premature separation and failure to rupture interferes with
delivery.
- The foal progressively becomes hypoxic, weak, and dead.
- This
condition should be treated as an emergency with rupture of the membrane
and delivery of the foal.
In any case, correction of dystocia should aim to
minimize trauma to the mare.
- Elevation of
the hindquarters with the mare under general anesthesia provides
additional room to manipulate the fetus.
- Fetotomy is a viable solution,
provided trained personnel and proper instruments are available.
Otherwise, trauma to the mare is likely.
- Caesarian section is an
excellent alternative if facilities and personnel are available.
- One of
the biggest problems with fetotomy or caesarian section is the delay in
making the decision to go forward with either option.
- If the decision is
delayed, the mare becomes exhausted and the reproductive tract
traumatized.
- The procedure and recovery then becomes more difficult.
- The
benefit of timely decision making is shown by studies examining elective
c-section in mares in which live foals were delivered, some mares had
repeat sections in following years, others had vaginal delivery and so
forth.
Induction of
parturition
- Induction of
parturition in mares had a bad reputation for years because of inability
to determine when the foal was mature enough for life outside the womb.
-
Induction of parturition based on gestation length alone or even with
the additional information of udder development and relaxation of the
ligaments and cervix resulted in the delivery of premature foals that
needed intensive care to survive and frequently died in spite of the
care.
- With the knowledge of the changes in mammary secretion
electrolytes, however, induction can now be performed safely.
- The
criteria to be met before induction include
- 330 d gestation minimum,
-
colostrum in the udder,
- relaxation of the ligaments and cervix and most
importantly,
- changes in the mammary secretions of >400 ppm (10 mmol)
calcium. This is the KEY CRITERIA.
- Inversion of the Na:K ratio is also
critical (K should be > Na in mammary secretions)
Methods of induction
- It
is advisable to place a jugular catheter before inducing parturition.
Oxytocin is the drug of choice.
-
The dose used is related to the intensity of parturition and the time to
delivery.
-
The smoothest induction is with a low dose (5-10 IU bolus IV
or 10 IU in 200 ml over 15 min).
-
The hypothesis is that a small dose
begins the cascade and the endogenous response carries it on.
-
Other
reported protocols include: single IM bolus (100 IU; 40-60 IU); multiple
small IV injections (10-20 IU) every 10 min; IV boluses (20-40 IU) in 60
ml saline every 20 min; IV drip (60-80 IU) in 500 ml saline; but
parturition is more rapid and forceful with these higher doses.
-
The
trend is toward smaller doses which seem more physiologic.
PGF2a is effective in inducing parturition but
results in an increase in premature placental separation, dystocia and
foal mortality. It is NOT recommended
Indications are that if criteria for induction are
met (including Ca level of mammary secretions), fluprostenol is safe and
effective but the time interval from treatment to parturition is longer
and more variable than oxytocin.
Steroids given repeatedly in high doses will
shorten gestation length but are ineffective for inducing parturition
for practical purposes.
Postpartum
disorders Retained
placenta
- Retained placenta is rare due to
the strong uterine contractions and microcotyledonary attachment of the
placenta in mares.
- Retention usually occurs in the non-gravid horn.
-
Unlike the cow, this should be treated as an emergency.
- Tissue breakdown
and bacterial growth may lead to metritis - laminitis - septicemia
complex.
- The placenta should be passed in 3 h, if not, initiate
treatment prior to 4 -6 h postpartum.
- The aims of treatment are to
stimulate release of the placenta, evacuate the uterus, encourage
involution, control bacterial growth and prevent laminitis.
-
Treatment
- Attempts to remove the placenta manually risk hemorrhage and
trauma to the uterus. Manual removal is not recommended.
- Prior to 4 - 6 h after
parturition
- Re-distension of chorio-allantois may be attempted (Burn's
technique)
- This
method is usually quite effective if there is only a single hole in the
placenta at the cervical star area.
- Insert tube into placenta
(not around it!) and distend with fluid (home
made isotonic saline is good)
- Distend placenta (stand
back when the fluid rushes out)
- Repeat until placenta
releases
 
 
 
- The more effective
oxytocin method is to administer the oxytocin in
an IV drip (50 IU) in 500 ml saline over a 30 min period (this is the '5
method'...... 50 units, 500 mL, 0.5 hours)
- Other methods
include a large IM bolus of 80-100 IU or small IV doses (10-20 IU)
repeated every 15 min.
- Always examine the placenta after passage to make
sure it is all present.
- It
is helpful to know the normal appearance to be able to identify
pathology.
- After 4 - 6 h
- Treatment should
include broad spectrum systemic antibiotics, e.g. potassium penicillin
(22,000 - 44,000 IU/kg, IV, QID) plus gentamicin (6.6 mg/kg, IV, SID)
plus metronidazole (15 mg/kg, PO, BID).
- In addition, uterine lavage with
saline will reduce the accumulation of debris in the uterus.
- The
retention should be manually re-evaluated, at least daily.
- Exercise is
helpful, provided there are no signs of laminitis.
- Make sure that
tetanus vaccination is current. If not, administer tetanus toxoid.
- Monitor the mare for signs of metritis - laminitis - septicemia complex.
Metritis - laminitis - septicemia
complex.
- This problem may develop due to
gross contamination at foaling or retained placenta.
- Affected mares
exhibit depression, anorexia, congested mucous membranes, elevated
temperature, pulse, and respiration rate.
- Signs appear as early as 12 h
postpartum.
- Treatment consists of evacuating the uterus by large volume
lavage (with saline) to eliminate debris and toxins.
- Systemic therapy
consists of systemic antibiotics, fluids, anti-inflammatories, tetanus
toxoid, monitoring for laminitis, etc. as outlined previously for
retained placenta.

Delayed uterine involution
- Normally,
involution in the mare is very fast.
- By 7 d postpartum the uterus is 2 -
3 times the size of the uterus of a barren mare.
- Mares with delayed
uterine involution may have a discharge, occasionally exhibit dullness
or mild pain and on rectal exam have a large, baggy, flaccid uterus.
-
Ultrasound exam reveals excessive fluid in the uterus.
- Treatment
consists of uterine lavage, oxytocin (50-100 U in 500 ml IV drip, or
multiple small doses), exercise (provided there are no signs of
laminitis), antibiotics, etc. Oxytocin therapy is especially important
in cases where the foal is dead because then the normal endogenous
release of oxytocin in response to suckling is absent.
Postpartum hemorrhage
- Hemorrhage
can occur into the broad ligament dissecting between the myometrium and
serosa.
- Clinical signs are characterized by a slow onset (12-48 h), with
signs of colic, sweating, pale mucous membranes and elevated pulse.
-
There may be no signs but a hematoma is found on the prebreeding exam.
-
Diagnosis is by rectal exam and ultrasonography, aided by
abdominocentesis.
- Treatment is basically supportive care and consists of
keeping the mare quiet and providing analgesics.
Uterine prolapse
- This
is a true emergency in the mare.
- Even with rapid attention, the
prognosis for survival is estimated as 50%.
- The uterus should be cleaned
and replaced as soon as possible.
- The vulva is not sutured as in the
cow.
- Treat the mare for shock if needed.
- Administer anti-inflammatories,
systemic antibiotics, tetanus toxoid, oxytocin.
Uterine tears
- The
most common location is dorsal, just anterior to the cervix.
- Initial
treatment is for hemorrhagic shock.
- Surgical repair is indicated, unless
the tear is small and dorsally located.
- They often lead to peritonitis.
-
Medical treatment consists of oxytocin (e.g. 20 IU every 2 h) and / or
ergonovine 1-3 mg i.m., repeated every 2-4 h., along with antibiotics,
and NSAID's.
- Massage per rectum after surgical repair is indicated to
prevent adhesion formation.
Recto-vestibular and perineal lacerations
-
These are more common in maiden mares due to a tight
vaginal-vestibular sphincter.
-
They also occur in cases of fetal
malpositioning, relative fetal oversize and overzealous assistance.
-
These will be covered more thoroughly in the surgery sessions.
-
Basically, immediate repair can be attempted but if not done immediately
after occurrence, repair should be delayed until the initial
inflammation has subsided.
Cervical laceration
- Trauma
to the cervix may interfere with its normal valve like action, affecting
its competency to permit breeding and maintain pregnancy.
- Damage is
often iatrogenic following dystocia or fetotomy.
- Treatment is surgical
repair bur because the surgery is difficult and often unsuccessful, a
BSE is recommended before surgery.
- Cervicitis / Vaginitis
- Necrotic vaginitis and/or cervicitis possible
after dystocia
- Can interfere with urination, defecation
(swelling, abscess formation)
- Treat with antibiotics, NSAIDs, Tetanus
toxoid

Gastrointestinal complications
-
Various complications can occur, including
constipation, small colon bruising, and rupture of the rectum, cecum, or
small colon.
-
Signs of colic and peritonitis follow.
-
The diagnosis can
often be confirmed with paracentesis.
Elective
termination of pregnancy
- Numerous
indications exist, with twinning and inadvertent breeding being some of
the most common.
- The choice of method depends greatly on the stage of
gestation.
- Before 5-7 d post ovulation there is no effective method. The
embryo has not entered the uterus yet and the CL is not responsive to
PGF.
- From 5 d post ovulation until the endometrial cups form at about 35
d, any number of methods will terminate pregnancy.
- Probably the simplest
is an injection of PGF.
- Uterine lavage or manual crushing will also end
the pregnancy.
- In the case of twins, where it is desired to maintain one
vesicle while destroying the other, isolation of one vesicle and manual
crushing is the preferred method.
- Because of the mobility of the early
vesicles, isolation and crushing is best performed before d 16.
- After
the endometrial cups have formed, PGF can still be used to terminate
pregnancy but multiple injections may be necessary.
- Uterine lavage or
uterine infusion can also be used, as well as manual crushing if it is
early enough to be able to grasp the vesicle.
- Various methods have been
employed to terminate one of a set of twins while allowing the other to
continue to term.
-
Currently one of the most promising is ultrasound
guided aspiration.
-
Although only about a third of mares treated with
this technique will carry the remaining foal to term, this is a much
higher percentage than would be successful if no intervention was
practiced.
-
Fetal
decapitation
at
about
75
days
is
the
best
method
to
terminate
twins.
-
Twin Reduction by Cervical Dislocation (as told by Karen Wolfsdorf)
-
Best time to perform surgery is between 75 to 85 days
-
Ultrasound to locate and identify fetuses, choose the one with the least surface area or closest to the tip of the horn
-
Give Banamine pre-op
-
Give 0.5 cc detomidine
-
Clip and give local block
-
Give another 0.5 cc detomidine
-
Give 1.0 cc propantheline (This is critical – if skip this, uterus will be too turgid to be able to perform task - available from HGD Pharmacy)
-
Grid incision (big enough to permit arm in abdomen)
-
Locate fetus, dislocate cervix by rolling between thumb and second finger (bigger fetuses – sort of like popping a cork on a bottle)
-
Routine closure
-
Post-Op Banamine q 12 h for 2 d
-
Double dose Regumate for 30 d
-
Pen/Gent for 3 d, then 7 more d of SMZ
|
 Equine
Index
Equine
Index